- Author Jason Gerald gerald@how-what-advice.com.
- Public 2023-12-16 10:50.
- Last modified 2025-06-01 06:05.
Menstrual pain is a very common problem experienced by 50-90% of women of reproductive age. Pain during menstruation is caused by muscle tension in the uterine wall. Strong and prolonged muscle contractions in the uterus will cause cramps. Cramps usually begin 1-2 days before menstrual bleeding occurs, and then disappear 1-2 days after the first day of your period. Generally, pain in the pelvis or lower abdomen feels sharp, intermittent, with varying intensity, but sometimes it is a persistent pain. Pain also sometimes radiates to the back, thighs, and upper abdomen. If the intensity of your pain is moderate to severe, you can reduce it with proven medical options, alternative medical therapies, natural remedies, diet, and physical activity.
Step
Method 1 of 4: Seeking Medical Help

Step 1. Take over-the-counter medications
Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen are the mainstays of treating menstrual pain. NSAIDs work by blocking the contractions that cause pain. The most widely used drug is ibuprofen. You can take ibuprofen 400-600 mg every 4-6 hours or 800 mg every 8 hours for a maximum dose of 2,400 mg a day.
- You should start taking the medication as soon as you have menstrual symptoms, and continue for 2-3 days as needed, depending on the pattern of symptoms. If you wait until after it's started, especially if you've had excruciating pain, you run the risk of experiencing pain so severe that nothing can be done about it.
- Try ibuprofen brands like Advil and Motrin. You can also try a naproxen brand like Aleve.

Step 2. Learn about hormonal contraception
If natural remedies, diet and nutrition, exercise, and NSAIDs don't provide satisfactory pain relief, hormonal contraception may be a good option to try. There are many types of contraceptives that are effective for reducing menstrual pain.
The method of choice is tailored to general health, sexual practices, and personal and financial preferences. Discuss the options with a medical professional

Step 3. Take birth control pills
Birth control pills are hormonal contraceptives that must be taken every day. Because you control when you take them, it's very easy to stop taking the pills. Birth control pills are used by many people, are easy to obtain, and relatively inexpensive. However, the use of pills is sometimes a bit inconvenient because they have to be taken every day at the same time.

Step 4. Use the KB patch
The patch works the same as pills, but in the form of a patch. The patch has to be worn for a week, and like pills, it's easy to stop.
Patches are also easy to come off, clearly visible when affixed to certain areas, and require constant monthly expenses

Step 5. Try a vaginal ring
If you don't want to use pills or patches, try a vaginal ring. This hormonal contraceptive only needs to be changed every month and it is easy to stop using it when it is no longer needed. Vaginal rings are considered more private than patches or pills because you don't need to take the pill or attach the patch for anyone to see.
The vaginal ring comes off easily during sexual intercourse and is also a constant monthly discharge

Step 6. Consider hormone injections
If you don't like the other options, try hormonal injections. This type of contraception is more convenient because it is only given every 3 months, but must be injected. However, the side effects are more detrimental than other options. Menstruation may stop and you may be infertile for up to a year after stopping the injection.
This option can lead to weight gain

Step 7. Try hormonal birth control in the form of implants
Implants are a permanent option for controlling menstrual pain. Once inserted, implants can last up to 3-5 years. Although they can be used for a long time, the implants are also easy to remove.
The implant insertion process is also sometimes painful, but only needs to be done once every few years. Implants can cause regular bleeding

Step 8. Consider an intrauterine device (IUD)
If you don't think implants are the right choice, try an option that can last even longer, namely the IUD. These contraceptives are effective for three to five years, and the side effects are small.
If you contract a sexually transmitted disease, your risk of pelvic infection increases within 30 days of inserting the IUD. Fertility returns as soon as the IUD is removed
Step 9. See a doctor
If your pain is more severe than usual, and if the timing or location of the pain is different, call your doctor. You should also consult a doctor if the pain lasts more than 2-3 days. There is a possibility that the pain is secondary dysmenorrhea, which is more severe than menstrual pain, the cause is another disease or disorder.
- There are certain reproductive disorders that cause secondary dysmenorrhea. These disorders include endometriosis, pelvic inflammatory disease, cervical stenosis, and tumors in the uterine wall.
- If your doctor suspects you have one of these disorders, they will perform a physical exam and tests to see if it is possible. The doctor will perform a pelvic examination and check for abnormalities or infections in the reproductive organs. You may have to undergo an ultrasound, CT scan, or MRI. In some cases, the doctor will perform a laparoscopy, which is an outpatient procedure that involves surgically inserting a camera into the body to examine the abdominal cavity and reproductive organs.
Method 2 of 4: Using Alternative Therapies and Natural Medicines

Step 1. Use heat
There are several natural therapies that have been researched and proven to help relieve menstrual pain. One of the most common and easy methods is to use heat. Heat is sometimes as effective or even more effective than over-the-counter pain relievers, such as ibuprofen or acetaminophen. Heat helps relax muscles that are tense due to pain. You should apply heat to your lower abdomen, or your lower back. Try a patch or heating pad. The heat patch for this use is non-medicated, only conducts heat for up to 12 hours. You can stick it to your skin or clothes, but read the instructions first.
- Hot patches come in different shapes and sizes for different uses, but you can use any one to relieve menstrual pain. There are several brands that produce special patches for menstrual pain, such as ThermaCare Heat Wraps.
- The use of the patch is easier than the heating pad because it is practical. So you can paste it anywhere and continue the activity.
- If you don't have a patch or heating pad, you can soak in a hot tub or take a hot shower to help relax your body and relieve pain.

Step 2. Try a behavioral intervention
It may be helpful to develop recovery strategies with specific behavioral interventions, especially if the pain is too severe. This strategy includes relaxation exercises that use repetitive activities, such as deep breathing, saying the same prayer, or repeating a word or sound, combined with clearing your mind, ignoring distractions, and being positive. This should help you relax and forget about the pain.
- You can also try imaginary interventions, which use positive thoughts and experiences to change emotional states and distract and relieve pain.
- Another method is hypnotherapy, which uses hypnosis to induce relaxation, reduce stress, and relieve pain.
- Since pain affects the same muscles for childbirth, there are some women who are helped by Lamaze exercises. Try the rhythmic breathing used in Lamaze exercises to relieve or reduce pain.
- You can also try biofeedback, which is a method to learn to control physiological parameters such as heart rate, blood pressure, temperature, and relaxation techniques to train your body to control your symptoms.
Step 3. Divert attention
Distraction is the easiest and most effective pain reliever. If you have intense pain, do something that would normally make you forget about your surroundings, such as socializing with good friends, reading a book, playing a computer game, watching TV or movies, or playing Facebook.
Make sure you choose an activity that distracts you from the pain and convinces your body to focus on something else
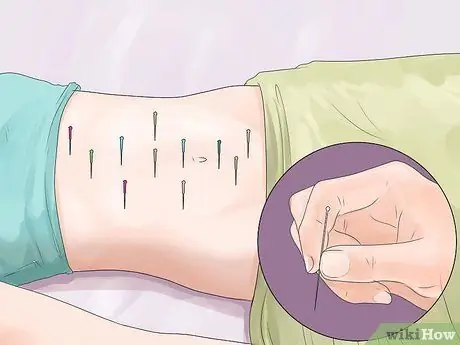
Step 4. Try acupuncture
Acupuncture has been practiced as a method of relieving pain since 2,000 years ago. This method inserts a hair-thin needle into the skin at a specific location. The needles are painless in most people, and some women feel their menstrual pain go away after a while.
Despite the many testimonies, studies on the efficacy of acupuncture have not found definitive conclusions

Step 5. Gently massage the abdomen
Sometimes, gentle pressure on the painful area is helpful. Lie down and lift your legs. From that position, gently massage the lower back and abdomen.
Make sure your pressure is not too hard. Do not let it become more painful, even though the goal is to relieve pain. This pressure can relax the muscles and relieve pain
Method 3 of 4: Using Diet and Nutrition

Step 1. Take supplements
Research shows that certain vitamin and nutritional supplements can reduce pain when taken daily. The mechanism is not well understood, but many dietary supplements have been shown to reduce pain. Take 500 U of vitamin E, 100 mg of vitamin B1, 200 mg of vitamin B6, and vitamin D in doctor-approved levels daily.
- Blood tests can assess whether you are getting enough of this vitamin in your diet, and the use of supplements follows the results of these tests.
- You can also take fish oil or cod liver oil supplements.

Step 2. Change your diet
There is one study that shows that a diet low in fat and rich in vegetables helps reduce menstrual pain. You should eat green vegetables that are rich in vitamins A, C, E, B, K, and folate. Just like supplements, these vitamins and minerals can reduce menstrual pain. Vegetables can also prevent anemia due to menstrual bleeding because vegetables are able to provide the nutrients needed to form new red blood cells.
- You also need to increase iron during menstruation. Eat red meat or take supplements to prevent anemia.
- Green vegetables and berries also contain antioxidants, which play a role in fighting inflammation associated with bloating.
- Another study showed that women who consumed 3-4 servings of dairy products had less pain during menstruation. However, don't overdo it if your stomach is prone to gas or bloating if you eat a lot of dairy products.

Step 3. Drink tea
There are various variants of tea that can reduce pain. When choosing a type of tea, choose a decaffeinated version so as not to affect its pain-relieving benefits. Raspberry, chamomile, and ginger teas have anti-inflammatory properties that help reduce pain.
- Caffeine-containing teas should be avoided because caffeine triggers anxiety and tension, which can make pain worse.
- There's no definite recommendation on how much tea to take for pain relief, but as long as it doesn't contain caffeine, you can enjoy it as much as you want.
- Drinking tea can also maintain adequate fluid in the body.

Step 4. Avoid alcohol and tobacco
Alcohol can cause water retention and bloating. Nicotine contained in tobacco can increase tension and cause constriction of blood vessels called vasoconstriction. This problem can reduce blood flow to the uterus and make the pain worse.
Method 4 of 4: Doing Physical Activity

Step 1. Exercise
Menstrual symptoms can generally be reduced with exercise, including pain. Exercise can release endorphins, which are natural pain relievers. Endorphins also fight the prostaglandins in the body that cause tension and pain. Therefore, physical activity can reduce pain and cramps.
Try different types of aerobic exercise, such as walking, running, biking, swimming, kayaking, hiking, or a gym class

Step 2. Perform simple stretches
Stretching helps relax muscles and reduce cramps. You can sit on the floor and stretch your legs. Stretch until you can reach your toes or ankles. Inhale while straightening your back. After a few breaths, lean toward the floor.
You can also try simple stretches to stretch your back or abdomen depending on the area that hurts the most

Step 3. Add sexual activity
Some women feel their pain subside during orgasm. The reason isn't very clear, but it may have something to do with the endorphins released during sexual intercourse. Just like exercise, the endorphins released during orgasm can relieve menstrual pain and inflammation.

Step 4. Try yoga
Similar to aerobic exercise and stretching, yoga helps relax the body and reduce aches and pains in the lower back, legs, and abdomen. If you start to experience menstrual pain, try different yoga poses. Before you start, wear comfortable clothes and pants, and put on some relaxing music.
- You can bend your body until your head reaches your knees. Sit on the floor and straighten your legs in front of you. Pull in one leg and bend it in 90 degrees so that the sole of the foot rests on the inside of the other thigh. Inhale and reach for your shins, ankles, or soles of your feet. Stretch your torso across your legs toward your feet. Exhale and lean down from above the thighs. Lengthen and stretch your back, don't bend it. Holding this pose while continuing to breathe, extend from the heels and press the sitting bones into the floor. Hold for 1-3 minutes, then switch to the other leg.
- You can also try the noose pose. Please sit crouched with your feet together. Lower the body position until the buttocks are close to the heels. Inhale, then move your knees to the left while rotating your torso to the right. As you exhale, roll your left arm behind your body until it's wrapped around your knee and leg. Inhale and reach for your right arm, then clasp both hands. Exhale, direct your gaze over your right shoulder. Hold for 30-60 seconds while breathing. Replace with the other side.
- You can also try camel pose. Get into a position on the floor with both knees supported, hips shoulder-width apart. Make sure your shins and instep are firmly pressed against the floor. Place your palms on your buttocks with your fingers pointing down. Inhale. Figure your chest and lower your shoulders toward your ribs. Exhale, then push your hips forward while arching your back back. To stabilize the position, place your hands on your heels. Raise your chest. Breathe steadily for 30-60 seconds.
Tips
- Try increasing the consumption of foods that contain potassium, such as bananas.
- Try prone or lying on your side with your knees under your body.
- Take longer showers. While it may not help if you're looking to conserve water, taking long showers can reduce stomach pain.
- If your pain is very severe or there seems to be a problem, see your doctor to discuss the symptoms. Pain may be a sign of another disease that needs to be treated, such as endometriosis, adenomyosis, uterine fibroids, pelvic inflammatory disease, congenital anomalies, or cancer.
- Other signs and symptoms that require medical attention are fever, vomiting, bleeding so much that it fills up a pad or tampon every two hours, dizziness or fainting, sudden or severe pain, pain that is different from normal menstrual cramps, pain when urinating urination, abnormal vaginal discharge, and pain during sexual intercourse.
- Try lying down and placing a hot water bottle on your stomach.
- Do not use an ice pack or anything cold.
- Always taking pain medication can harm the lining of the stomach wall. Overuse of the drug can also cause diarrhea, and the body will become resistant to the pill.
- Try lying on your back and raise yourself in a Bridge position. This will stretch the abdominal muscles.
- Take medicine and try to sleep/relax. The medicine will start to work when you relax so that the tension in the body is reduced.






