- Author Jason Gerald gerald@how-what-advice.com.
- Public 2023-12-16 10:50.
- Last modified 2025-01-23 12:04.
An aneurysm occurs when a blood vessel in an artery enlarges or swells due to injury or weakening of the artery wall. Aneurysms can occur anywhere, but are most common in the aorta (large artery that originates in the heart) and the brain. The size of an aneurysm varies depending on the factors that caused it, such as trauma, medical conditions, genetics, or congenital conditions. If it continues to grow, the aneurysm is more likely to rupture and cause heavy bleeding. Most anerusimes are asymptomatic and have a high mortality rate (between 65%-80%), so you should seek immediate medical attention.
Step
Method 1 of 4: Detecting a Cerebral Aneurysm

Step 1. Don't underestimate a sudden, severe headache
If an artery ruptures in the brain due to an aneurysm, you may experience severe headaches that come on suddenly. This headache is a key symptom of a ruptured brain aneurysm.
- Usually a headache will feel worse than a headache you've had before.
- The headache is usually only felt in one area, limited to the side of the head with a ruptured artery.
- For example, if the ruptured artery is near your eye, you may experience a severe headache that radiates to the eye.
- Headaches may also be associated with nausea and/or vomiting.

Step 2. Watch for visual disturbances
Double vision, decreased vision, blurred vision, or blindness are indicators of a cerebral aneurysm. Impaired vision occurs due to pressure on the walls of the arteries near the eye that blocks blood flow to the eye.
- The optic nerve can also be pinched due to accumulated blood causing blurred or double vision.
- Blindness is caused by retinal ischemia, which is a condition caused by insufficient blood flow to the retinal tissue.

Step 3. Look in the mirror to see if your pupils are dilated
An enlarged pupil is a common sign of a cerebral aneurysm caused by a blocked artery near the eye. Usually, one pupil will appear larger.
- Dilated pupils are caused by blood pressure that accumulates in the brain.
- Dilated pupils may be an indication that an aneurysm has recently occurred, indicated by damage to the arteries near the eye.

Step 4. Watch for eye pain
Your eye may throb or feel intense pain during the aneurysm.
- This occurs when the ruptured artery is near the eye.
- Eye pain is usually one-sided because it is only felt in the part of the brain that is experiencing the aneurysm.

Step 5. Notice if your neck is stiff
A stiff neck may be due to an aneurysm if the nerves in the neck are affected by a ruptured artery.
- A ruptured artery doesn't always have to be near the area of the neck that hurts.
- This is because the nerves of the neck extend quite far up and down the neck and head area.

Step 6. Feel if one side of your body feels weak
Weakness on one side of the body is a common sign of an aneurysm, depending on which part of the brain is affected.
- If the right side of the brain is affected, the left side of the body is paralyzed.
- Conversely, if the left side of the brain is affected, the right side of the body is paralyzed.

Step 7. Seek immediate medical attention
Ruptured brain aneurysms are fatal in about 40% of sufferers, and about 66% who make it through suffer some form of brain damage. If you experience any of the above symptoms, call an ambulance immediately.
Experts do not advise patients to drive their own car or be escorted by family members to the hospital. Aneurysms can react quickly and paramedics must perform surgical procedures on the patient in the ambulance
Method 2 of 4: Detecting Aortic Aneurysms
Step 1. Recognize that there are two types of aortic aneurysms: abdominal aortic aneurysms and thoracic aortic aneurysms
The aorta is the main artery that delivers blood to the heart and all the limbs, and aneurysms affecting the aorta can be classified into two subtypes:
- Abdominal aortic aneurysm (AAA). Aneurysms that occur in the abdominal area (abdomen) are called abdominal aortic aneurysms. This is the most common type of aneurysm and is fatal in 80% of cases.
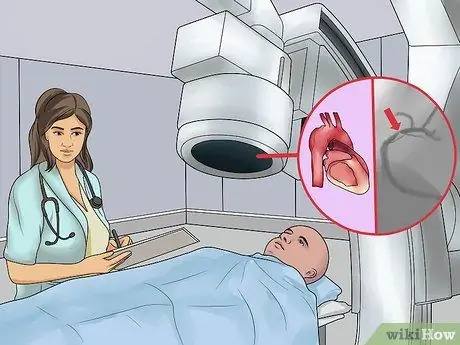
- Thoracic aortic aneurysm (AAT). This type of aneurysm is in the chest area and occurs above the diaphragm. During AAT, the passage near the heart enlarges and affects the valve between the heart and the aorta. When this happens, the blood flow in the heart is reversed and causes damage to the cardiac muscles.

Step 2. Watch for severe abdominal or back pain
Unusual and sudden severe abdominal or back pain may be a symptom of an abdominal aortic aneurysm or a thoracic aortic aneurysm.
- The pain is caused by enlarged arteries pressing on nearby organs and muscles.
- The pain usually doesn't go away on its own.

Step 3. Watch for nausea and vomiting
If you have nausea and vomiting along with abdominal or back pain, you may have a ruptured abdominal aortic aneurysm.
You may also experience constipation and difficulty urinating

Step 4. Check if you are dizzy
Headache is caused by the massive blood loss that often accompanies rupture of an abdominal aortic aneurysm.
Dizziness can also cause fainting

Step 5. Check your heart rate
A sudden increase in heart rate is a reaction to internal blood loss and anemia caused by rupture of an abdominal aortic aneurysm.

Step 6. Feel if your skin is sweating
Sweaty skin is said to be one of the symptoms of abdominal aortic aneurysm.
This occurs because an embolus (blood clot) is formed by an abdominal aneurysm and affects the surface temperature of the skin

Step 7. Watch for chest pain and sudden high-pitched wheezing
Because a thoracic aortic aneurysm occurs in the chest area, an enlarged aorta can poke into the chest area, causing pain and a loud sound when breathing.
- This chest pain is intense and stabbing.
- Chest pain that is not sharp may not be a symptom of an aneurysm.
Step 8. Feel if you have difficulty swallowing
Difficulty swallowing may be an indication of a thoracic aortic aneurysm.
Swallowing problems can occur because the enlarged aorta presses on the esophagus, making it difficult for you to swallow

Step 9. Listen for hoarseness in your voice
The enlarged arteries can press on the laryngeal nerves, including the vocal cords, which makes a hoarse voice.
Hoarseness occurs suddenly, not gradually as with a cold or flu
Method 3 of 4: Confirming with Diagnosis
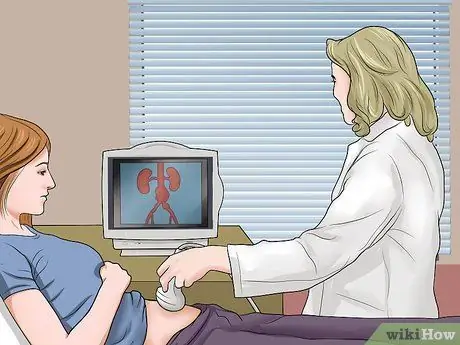
Step 1. Have an ultrasound to get a preliminary diagnosis
Ultrasound is a painless procedure that uses sound waves to visualize and create pictures of certain body parts.
This test can only be used to diagnose an aortic aneurysm
Step 2. Try a computed tomography scan (CT-Scan)
This procedure uses X-rays to take photos of structures inside the body. A CT scan is a painless procedure and provides more detailed images than ultrasound. This is a good choice if the doctor suspects an aneurysm or wants to exclude the possibility of other diseases.
- During the procedure, the doctor will inject a dye into the blood vessels that make up the aorta and other arteries that are visible on a CT scan.
- This procedure can be used for the diagnosis of all types of aneurysms.
- You can have a CT scan as part of a routine checkup even if an aneurysm is not suspected. This procedure is good for identifying the aneurysm as early as possible.
Step 3. Consider a magnetic resonance imaging (MRI) test
This procedure uses magnets and radio waves to visualize organs and other structures in the body. This procedure is also painless and is used to detect, locate, and measure aneurysms.
- This procedure can produce 3D photos of the hemispheres of blood vessels in the brain.
- MRI can be used to diagnose all types of aneurysms.
- In some cases, MRI and cerebral angiography may be used together to support each other.
- Using radio waves and computer-generated magnetic fields, MRI can produce more detailed images of the blood vessels of the brain than CT scans.
- This procedure is safe and painless.
- Unlike X-rays, MRI does not use radiation and is safe for use by people who avoid radiation, such as pregnant women.
Step 4. Try angiography to examine the inside of the artery
This procedure uses X-rays and special dyes to visualize the inside of the aneurysm of the artery.
- This will show the extent and severity of arterial damage, plaque buildup and arterial blockages can be seen easily with the help of this procedure.
- Cerebral angiography is only used to detect cerebral aneurysms. This procedure is invasive because it uses a small catheter that is inserted into the leg and guided through the circulatory system.
- This procedure will show the exact location of the ruptured artery in the brain.
- After the dye is injected, a series of MRIs or X-rays will then follow to create detailed photos of the brain's blood vessels.
Method 4 of 4: Understanding Aneurysms
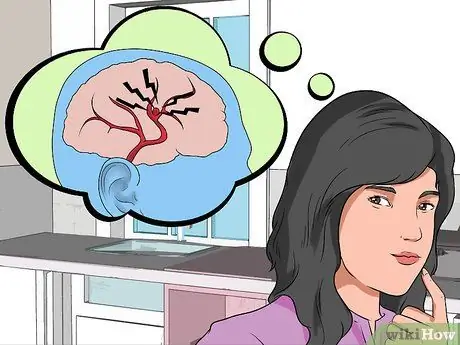
Step 1. Understand the causes of cerebral aneurysms
A cerebral aneurysm occurs when an artery in the brain weakens and forms a bubble before it bursts. Bubbles usually form in the fork or branch of an artery which is the weakest part of the blood vessel.
- When the bubble bursts, persistent bleeding in the brain will occur.
- Blood is toxic to the brain, and when bleeding occurs, the condition is usually called hemorrhagic syndrome.
- Most brain aneurysms occur in the subarachnoid space, which is the area between the brain and the skull.

Step 2. Know your risk factors
Cerebral and aortic aneurysms share several risk factors in common. Some are uncontrollable, such as inherited genetic conditions, but other factors can be reduced by smart lifestyle choices. Here are some common risk factors for cerebral and aortic aneurysms:
- Smoking increases the risk of both types of aneurysms above.
- Hypertension, or high blood pressure, damages blood vessels and the lining of the aorta.
- Increasing age increases the risk of cerebral aneurysm after age 50. The aorta becomes stiffer with age, and the likelihood of aneurysm increases with age.
- Inflammation can cause damage that leads to an aneurysm. Conditions such as vasculitis (inflammation of the blood vessels) can damage and scrape the aorta.
- Trauma, such as a fall or motor vehicle accident, can damage the aorta.
- Infections such as syphilis (a sexually transmitted disease) can damage the lining of the aorta. Bacterial or fungal infections in the brain can damage blood vessels and increase the risk of an aneurysm.
- Use or abuse of illicit substances, especially cocaine and excessive alcohol, causes hypertension which can lead to brain aneurysms.
- Gender plays a role in aneurysm risk. The risk of aortic aneurysm in men is higher than in women, but women have a higher risk of brain aneurysm.
- Certain inherited conditions, such as Ehlers-Danlos syndrome and Marfan syndrome (both are connective tissue disorders), can cause weakening of the cerebral blood vessels and the aorta.

Step 3. Quit smoking
Smoking is believed to have contributed to the formation and rupture of brain aneurysms. Smoking is also the most significant risk factor for abdominal aortic aneurysm (AAA). 90% of patients with aortic aneurysm have a history of smoking.
The sooner you quit, the sooner you can start lowering your risk

Step 4. Pay attention to blood pressure.
Hypertension, or high blood pressure, can damage the cerebral blood vessels and the lining of the aorta which then leads to the development of an aneurysm.
- If you are overweight or obese, losing weight can reduce blood pressure. A reduction of 5 kg can make a difference.
- Exercise regularly. 30 minutes of moderate physical exercise a day can help lower blood pressure.
- Limit alcohol. Do not drink more than 1-2 drinks per day (1 for women, 2 for men).
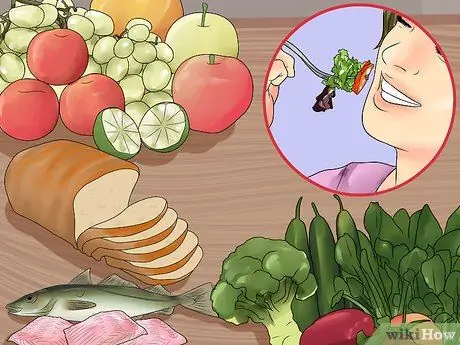
Step 5. Manage your diet
Maintaining healthy blood vessels can help avoid aortic aneurysms. A healthy diet can help reduce the risk of rupture of an existing aneurysm. A balanced diet with lots of fresh fruit and vegetables, whole grains, and lean protein will help prevent aneurysm from forming.
- Reduce sodium. Limiting sodium to less than 2,300 mg daily (1,500 mg daily for people with a diagnosis of active high blood pressure) will help control blood pressure.
- Lower cholesterol. Eating foods high in soluble fiber, especially oatmeal and oat bran, will help reduce “bad” (LDL) cholesterol. Apples, pears, kidney beans, barley, and dried prunes also contain soluble fiber. Omega 3 fatty acids from fatty fish such as sardines, tuna, salmon, or halibut also help reduce the risk.
- Eat healthy fats. Make sure you avoid saturated fat and trans fat. Fats from fish, vegetable oils (eg olive oil), nuts, and seeds are high in monounsaturated and polyunsaturated fats, which can reduce risk. Avocados are another source of “good” fats that can help lower cholesterol.






