- Author Jason Gerald gerald@how-what-advice.com.
- Public 2024-01-19 22:11.
- Last modified 2025-06-01 06:05.
A damaged liver produces new tissue to heal itself, but a cirrhotic liver is unable to recover properly because its tissue begins to be replaced by connective fibers, so its structure changes. Early-stage cirrhosis can be treated with treatment of the underlying cause, but late-stage cirrhosis is usually incurable and requires a liver transplant. If left untreated, cirrhosis can lead to liver failure and/or cancer. Recognizing the signs of cirrhosis can help you detect the condition in its early stages, which can be treated.
Step
Method 1 of 4: Understanding the Risk Factors
Step 1. Think about the amount of alcohol you drink
Alcohol damages the liver by blocking its ability to process carbohydrates, fats, and proteins. When these substances build up to damaging levels, the body can react with reactive inflammation leading to hepatitis, fibrosis, and cirrhosis. However, excessive alcohol abuse is not the only thing that causes liver disease. Only 1 in 5 heavy drinkers develop alcoholic hepatitis, and 1 in 5 people develop cirrhosis.
- Men are considered "heavy drinkers" if they consume more than 15 drinks a week. Women are considered "heavy drinkers" if they consume 8 or more servings of drinks a week.
- You can still get cirrhosis after you stop drinking. However, abstinence from alcohol is still recommended for all people with cirrhosis. This step will help with the treatment and healing process, no matter what stage of cirrhosis you have.
- Although cirrhosis is more common in men, cirrhosis in women is more likely to result from alcoholism.
Step 2. Get tested for hepatitis B and C
Inflammation and chronic liver injury from these two viruses can progress to cirrhosis within decades.
- Risk factors for hepatitis B include unprotected sex, blood transfusions, and injections with contaminated needles. These cases are less common in the US and other developed countries because their vaccination systems are good.
- Risk factors for hepatitis C include infection from needles to drugs, blood transfusions, and body piercing and tattoos.
- Cirrhosis from hepatitis C is the predominant reason for liver transplantation.

Step 3. Study the correlation between cirrhosis and diabetes
15-30% of people with cirrhosis develop their diabetes condition into "non-alcoholic steatohepatitis" (NASH) syndrome. Diabetes is also common in people with hepatitis C - which is a common cause of cirrhosis - mainly due to decreased pancreatic function.
- Another cause of cirrhosis that is often associated with diabetes is hemochromatosis.
- This condition is characterized by iron deposits in the skin, heart, joints, and pancreas. Its buildup in the pancreas causes diabetes.

Step 4. Consider your current body weight
Obesity poses many health risks, from type 2 diabetes and heart disease, to arthritis and stroke. However, excess fat in the liver causes inflammation and damage that can develop into the condition NASH.
- To determine if your body weight is within a healthy range, use an online body mass index (BMI) calculator.
- BMI calculation takes into account age, height, gender, and body weight.

Step 5. Know your risk for autoimmune and heart diseases
If you have an autoimmune disease such as inflammatory bowel disease, rheumatoid arthritis, or thyroid, be careful. Although all of these diseases do not directly contribute to cirrhosis, the risk of complications from medical disorders increases, which can lead to cirrhosis. Heart disease is a risk factor for the condition NASH, which can lead to cirrhosis. In addition, heart disease on the right side can cause liver nutmeg and heart cirrhosis.
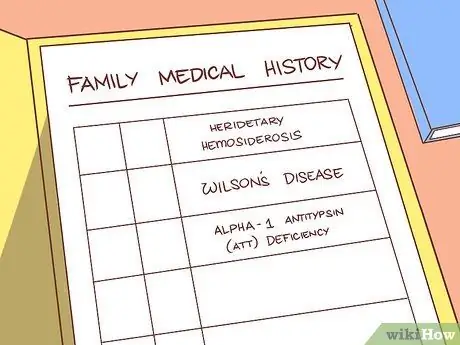
Step 6. Check the family history
Some types of liver disease that can cause cirrhosis have a genetic hereditary pattern. Look at the family medical history for diseases that pose a high risk for cirrhosis:
- Hereditary hemosiderosis
- Wilson's disease
- Deficiency of alpha-1 antitrypsin (AAT)
Method 2 of 4: Recognizing the Symptoms and Signs

Step 1. Recognize the symptoms of cirrhosis
If you experience it, see a doctor immediately. He or she can provide a professional diagnosis and immediately begin the treatment process. If you're trying to find out if someone else has cirrhosis, make sure you take them in for an evaluation, as they may have subtle symptoms. These symptoms include:
- Fatigue
- Easy bruising or bleeding
- Low-grade edema (swelling)
- Yellow skin and eyes (jaundice)
- Fever
- Decreased appetite or body weight
- Nausea
- Diarrhea
- Intense itching (pruritus)
- Increased abdominal circumference
- Confusion
- Sleep disturbance

Step 2. Look for the condition of spider veins
The technical terms are spider angiomata, spider nevi, or spider telangiectasias. Spider veins are abnormal collections of veins that arise from injured central veins. Spider veins usually occur on the trunk, face, and upper arms.
- To verify, press the glass over the collection of veins you suspect.
- The red dot in the center of these clusters will appear to be throbbing - reddening as the blood enters, then blanching as the blood moves into the smaller veins.
- Large spider angiomas in high enough numbers are a sign of more severe cirrhosis.
- However, this condition also often occurs in pregnant women or people who are malnourished. Sometimes, healthy people can have it too.

Step 3. Observe the redness of the palms
Palmar erythema looks like red dots on the palms, and is caused by changes in sexual hormone metabolism. Palmar erythema usually affects the outer margin of the palm along the thumb and little finger, and does not affect the center.
Some causes of palmar erythema include pregnancy, rheumatoid arthritis, hyperthyroidism, and blood problems
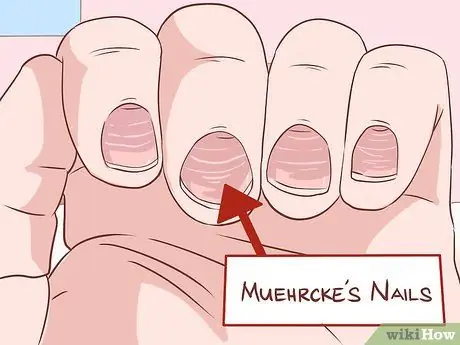
Step 4. Look for any changes to the nails
Liver disease usually affects the skin, but you can get useful additional information by observing your nails. Muehrcke's syndrome occurs when there are pale horizontal stripes on the nail bed. This is the result of a lack of albumin production, which comes from the liver. Pressing on the nails that have this syndrome will make the lines disappear and then reappear quickly.
- Terry nail is a condition in which the two thirds of the nail plate closest to the fist appears white. The remaining third of the part that is close to the fingertips is red. This condition is also caused by low albumin.
- Clubbing is a state of rounding / enlargement of the nail bed and fingertips. When this condition is severe, your fingers will look like the bottom of a chicken thigh, hence the term "drumstick fingers." This is more common in biliary cirrhosis.

Step 5. Examine the long bone joints for swelling
If you notice recurring swelling in your knees or ankles, this may be a sign of "hypertrophic osteoarthropathy" (HOA). The joints of the fingers and shoulders may also develop arthritis. This is the result of chronic inflammation of the connective tissue that surrounds the bone, so it can be very painful.
Be aware that the most common cause of HOA is lung cancer, so this should not be taken into account

Step 6. Find the curved radius
"Dupuytren's contracture" is a thickening and shortening of the palmar fascia - the tissue that connects the various parts of the palm. This situation then causes problems with finger flexibility, so that the finger will curve permanently. The fingers that suffer the most are the ring finger and little finger, and they usually feel sore, itchy, or painful. Patients will have difficulty holding objects, because this condition affects grip strength.
- Dupuytren's contracture is common in alcohol-induced cirrhosis, accounting for 1/3 of all cases.
- However, you can also find it in smokers, alcohol users who do not have cirrhosis, workers who use their hands in repetitive motions, and people with diabetes mellitus and Peyronie's disease.
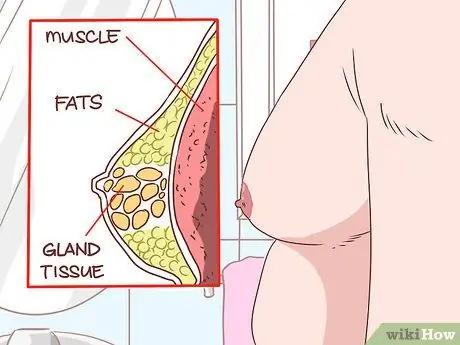
Step 7. Find a significant mass in the man's chest
Gynecomastia is the growth of glandular tissue on the male chest that extends from the nipple. This results in an increase in the hormone estradiol, and occurs in 2/3 of all cases of cirrhosis. Gynecomastia may look like pseudogynecomastia, which occurs due to fat instead of glandular growth.
- To tell the difference, lie on your back and place your thumb and index finger on each side of your chest.
- Press until both chests come together. You should look for a concentrated tissue sensation with a rubbery texture just below the nipple area.
- If you feel it, it means you have gynecomastia. Otherwise, you have pseudogynecomastia.
- Other mass abnormalities such as cancer usually occur separately (not centered around the nipple).

Step 8. Observe the symptoms of hypogonadism in men
Men with chronic liver problems such as cirrhosis may suffer from decreased levels of testosterone production. Symptoms of hypogonadism include impotence, infertility, loss of sexual desire, and shrinking of the testicles. Injury to the testicles or problems with the hypothalamus or pituitary gland can also be triggers.

Step 9. Watch for pain and swelling in the abdomen
Both of these symptoms can be a sign of ascites, which is a buildup of fluid in the peritoneal (abdominal) cavity. If enough fluid has accumulated, you may have difficulty breathing.
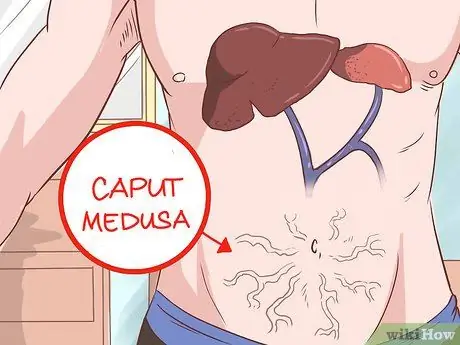
Step 10. Examine the abdomen for visible veins
Caput medusa is a condition where the umbilical vein opens, allowing blood to return to the portal venous system. This blood returns to the umbilical vein, where it flows into the abdominal wall veins. This causes the veins to be easily visible in the abdomen. This state is called caput medusa, because it depicts the head (caput) of Medusa, the goddess of Greek mythology.

Step 11. Try smelling your breath to detect an unpleasant smell
It denotes "fetor hepaticus" and is caused by some cases of severe hypertension causing the caput medusa as well as the Cruveilhier-Baumgarten state. This aroma is produced by the amount of dimethyl sulfide as a result of hypertension.
The sound of Cruveilhier-Baumgarten syndrome will be quieter as the doctor flattens the blood vessels by applying pressure to the skin above the belly button

Step 12. Notice the yellow eyes and skin
Jaundice is a condition that causes a yellowish discoloration due to an increase in bilirubin when the liver cannot process it effectively. The mucous membranes may also turn yellow, and your urine will darken.
Yellow skin is also caused by excessive consumption of carotene through carrots. However, carrots will not turn the whites of the eyes yellow like jaundice

Step 13. Examine the hand for asterixis
Ask the person you think has cirrhosis to stretch their arms fully out in front of the body, with the palms flat and facing down. The person's hands will move and “flap” around the wrist like the wings of a bird.
Asterixis also occurs in patients with uremia and chronic heart failure
Method 3 of 4: Request a Medical Expert Diagnosis
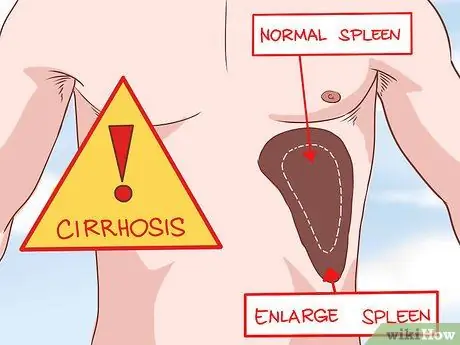
Step 1. Have your doctor check for changes in your liver or spleen size
When investigated, a cirrhotic liver will feel rough and swollen. Splenomegaly (enlargement of the spleen) is caused by high blood pressure, which results in compression of the spleen. Both of these conditions are symptoms of cirrhosis.

Step 2. Have the doctor examine Cruveilhier-Baumgarten's moaning sound
Most general care physicians will not examine this condition, which involves buzzing in the veins. This hum can be heard through a stethoscope in the epigastric (upper middle) region of the abdomen. Like caput medusa, it can also be caused by a condition where the different venous systems of the body connect - especially when the pressures are high.
The doctor will perform the Valsalva maneuver - which is an examination technique that increases pressure on the abdomen. This technique allows him to hear the sound more clearly if there is one

Step 3. Allow the doctor to run a blood test for cirrhosis
He or she may draw blood and run lab tests to diagnose cirrhosis. These tests may include:
- A comprehensive blood test for anemia can count leukopenia and neutropenia cells and detect the thrombocytopenia situation that is common in people with cirrhosis, among other things.
- Do a test to measure the level of the enzyme aminotransferase, which could indicate alcoholic cirrhosis. Alcoholic cirrhosis usually has an AST/ALT ratio greater than 2.
- Measure total bilirubin to compare with a healthy baseline level. The results may be normal in the early stages of cirrhosis, but tend to increase as the cirrhosis progresses. Be aware that elevated bilirubin is a poor prognostic sign in primary biliary cirrhosis.
- Measure albumin level. Liver with cirrhosis and failure to function may not be able to produce albumin. However, this condition also often occurs in patients with chronic heart failure, patients with nephrotic syndrome, malnutrition, and several other intestinal diseases.
- Other tests include alkaline phosphatase, gamma-glutamyl transpeptidase (GGT), prothrombin time, globulins, serum sodium, and hyponatremia.

Step 4. Ask your doctor to do a comparative image study to help identify cirrhosis
However, this study is more useful for detecting complications of cirrhosis such as ascites.
- The method of examination with ultrasound is noninvasive and is available in various places. Liver cirrhosis will look small and swollen. The right hemisphere of the liver can also be deflated while the left is enlarged. Liver nodules seen on ultrasound may or may not be harmful and require a biopsy. Ultrasound can also detect the diameter of the portal vein or the presence of collateral veins indicating portal hypertension.
- Computed tomography is not routinely performed for cirrhosis, because the information generated is the same as that of the ultrasound method. In addition, radiation and contrast exposure are required. Look for additional opinions and reasons the doctor recommends this process.
- The use of MRI is limited for reasons of cost and patient intolerance, as the process can be time-consuming and uncomfortable. Low signal intensity on T1-weighted images indicates the presence of iron overload due to hereditary hemochromatosis.

Step 5. Perform a definitive diagnostic biopsy
Symptoms and signs and blood tests are good methods of confirming suspected cirrhosis. However, the only way to know if your liver has cirrhosis is to have your doctor examine it for a biopsy. After processing and examining the liver sample under a microscope, the doctor can determine whether the patient has cirrhosis or not.
Method 4 of 4: Undergoing Cirrhosis Treatment

Step 1. Ask the medical staff for directions
Mild to moderate cases of cirrhosis are treated on an outpatient basis, with a few exceptions. If the patient has major gastrointestinal bleeding, severe infection with sepsis, renal failure, or is mentally disturbed, he or she should be hospitalized.
- Your doctor may ask you to stay away from alcohol, narcotics, and drugs if you have liver poisoning. He will evaluate it based on personal conditions. Some herbs such as kava and mistletoe can also cause further damage to the liver. Discuss all herbal/alternative treatments you are currently undergoing with your doctor.
- Doctors will provide immunizations against pneumococcal disease, influenza, and hepatitis A and B.
- The doctor will also run the NASH protocol for you. You will be made a plan for weight loss, exercise, and optimal control of lipid and glucose levels (fats, sugars/carbohydrates).

Step 2. Take medication as directed
As discussed in the previous sections, there are many causes that lead to cirrhosis. The treatment that the doctor prescribes will also be made specifically for your individual case. These drugs will treat the source of the disease (Hepatitis B, C, biliary cirrhosis, etc.) in addition to the symptoms stemming from cirrhosis and acute liver failure.

Step 3. Prepare for surgery
Your doctor doesn't always recommend it, but he or she can ask you to follow the procedure if some conditions occur as a result of cirrhosis. These conditions include:
- Varicose veins, or dilated veins, can be treated with ligase (surgically tying the blood vessels together).
- Ascites, a buildup of abdominal fluid that is treated by a paracentesis procedure.
- Fulminant hepatic failure, i.e. rapid development of encephalopathy (adjustment of brain structure/function within 8 weeks after detectable cirrhosis). This condition requires a liver transplant.
- Hepatocellular carcinoma is the development of liver cancer. Trial treatments include radiofrequency ablation, resection (surgery to remove carcinoma), and liver transplantation.

Step 4. Understand your prognostic procedure
After a diagnosis of cirrhosis, people can usually live for 5-20 years with or without symptoms. Once severe symptoms and complications appear, death within 5 years without a transplant is common.
- Hepatorenal syndrome is one of the severe complications that can occur as a result of cirrhosis. This syndrome is the development of renal failure in patients with liver disease. Patients should get medical treatment for cases of kidney failure.
- Hepatopulmonary syndrome, another serious complication, is caused by widening of the arteries in the lungs of people with liver disease. This condition results in shortness of breath and hypoxemia (low oxygen levels in the blood). The patient should be given a liver transplant.
Tips
- Do not take any medicines until your doctor prescribes them. Take care of the body with vitamins/juices/fruits.
- The early stages of cirrhosis can be treated by addressing the root cause, such as curbing sugar consumption for diabetics, avoiding alcohol, treating hepatitis, and changing obesity back to a normal weight state.






