- Author Jason Gerald gerald@how-what-advice.com.
- Public 2024-01-19 22:11.
- Last modified 2025-01-23 12:04.
Incontinence in men is a symptom of many other syndromes and diseases that should be investigated. If you suffer from it, you may have nerve or genitourinary system problems or other syndromes. The key to preventing this disease from reoccurring is to determine what caused it beforehand. Try to recall any changes to your life that have occurred-such as taking a new medication-that could have caused these problems or added additional strain to the bladder. Various preventive measures can be applied to people who have not suffered from it. If you are currently experiencing it, start treatment by consulting a doctor.
Step
Method 1 of 5: Steps to Prevent Recurrent Incontinence

Step 1. Identify the types of incontinence that you can prevent
Many of the causes of this disease are, unfortunately, uncontrollable. Examples: benign prostatic hypertrophy, neurological disorders, stroke, prostate or bladder cancer, and many more. However, you can still take certain steps to reduce your risk of developing the disease.

Step 2. Quit smoking
One very effective way to reduce the risk of developing incontinence is to quit smoking. The National Health Institute of the United States reports that 50% of bladder cancer is caused by smoking. Pressure on the bladder caused by the tumor will result in incontinence. If you need help quitting smoking, schedule an appointment with your doctor for a consultation. Currently, there are several medications available to help you quit smoking.
Step 3. Lose weight to prevent incontinence
If you are overweight, extra pressure will be placed on your bladder. This will lead to incontinence. Although weight loss may sound difficult, if you do it successfully, the results will be worth it. Start by exercising more and eating nutritious foods. Other ways to help lose weight include:
- Make sure you get a healthy intake of protein, fruits, vegetables, low-fat dairy products, and carbohydrates every day. The daily intake for each of these food groups will depend on your weight, age, and health. If you must consume 2000 calories per day, eat six to eight servings of carbohydrates, four to five servings of vegetables, four to five servings of fruit, 0.09 to 0.20 kg of protein, two to three servings of low-fat dairy products, and two to three servings of oils and fats.
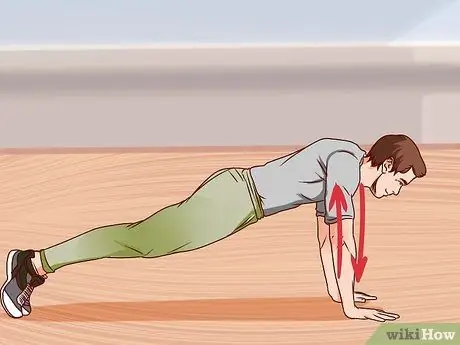
- Perform regular exercise that consists of cardiovascular exercises (running or swimming), lifting weights (such as push-ups or weightlifting), and flexibility (yoga or stretching).
- Limit the portion you eat each day.
- Choose low-calorie snacks such as fruits and vegetables.

Step 4. Increase your zinc intake
Research indicates that men with prostate cancer have 62-75% reduced levels of zinc in malignant prostate cells and that zinc plays a role in the malignancy of prostate cells. Zinc supplements are recommended for consumption; however, the level of intake is still unclear until now. Therefore, consult with your doctor about the amount of zinc supplements your body needs based on the zinc levels that are already in your daily menu.

Step 5. Increase lycopene intake
Lycopene is a powerful phytonutrient and antioxidant that has been shown to fight cancer. The five foods that have the highest levels of lycopene per cup are:
- Guava: 8587 uq
- Watermelon: 6889 uq
- Tomatoes: 7298 uq
- Papaya: 2651 uq
- Wine: 2611uq

Step 6. Eat more soybeans
Recent research has shown that the isoflavonoids contained in soybeans can help prevent prostate cancer. You can increase the amount of soy in your diet with edamame, soy milk, or tofu.
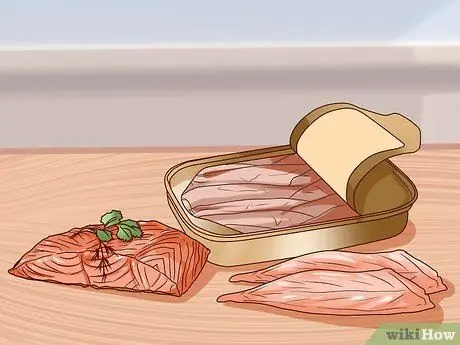
Step 7. Add more omega-3 fatty acids to your diet
Omega-3 fatty acids are found in various types of fish and other seafood such as salmon, mackerel, sardines, and sea bass. Research has shown that omega-3s can protect you from breast, colon, and prostate cancers.

Step 8. Maintain body water content
Drink at least eight glasses of water per day to prevent urinary tract infections, constipation, and kidney stones that can cause incontinence. You should drink as much as possible during the day and limit the number of drinks at night before bed.

Step 9. Set a time to the restroom
If you think you are suffering from incontinence, you can exercise your bladder to some degree. Schedule specific times to go to the restroom. This can exercise the bladder and prevent incontinence.

Step 10. Avoid foods and drinks that cause incontinence
Examples of substances that can cause incontinence are alcohol, caffeine, acidic, spicy foods, and sugar or artificial sweeteners.
- Alcohol is a diuretic, a substance that can cause the body to lose fluids. Alcohol also irritates the bladder and causes incontinence. Limit your alcohol intake to just one drink per night.
- Caffeine is also a diuretic. Limit drinking caffeine only in the morning.

Step 11. Try doing Kegel exercises
Kegel exercises are a good way to prevent incontinence by strengthening the pelvic floor muscles. This exercise is a bit tricky to learn because you need to be able to isolate the pelvic muscles, the part you use when you're trying to stop urine in the middle of the process. You will see or feel your testicles lift as you squeeze your pelvic muscles.
After you isolate the pelvic muscles, squeeze and hold for five seconds. Then, relax for five seconds. Repeat ten times with three sessions per day

Step 12. Avoid diuretics
Diuretic substances are drugs that are able to remove excess fluid from the body. This drug is usually prescribed for patients who have heart disease. Unfortunately, these drugs also have a tendency to cause incontinence. Some types include thiazide diuretics, loop diuretics, low potassium, and quinazoline. Examples of commonly used diuretic drugs are:
- Thiazide diuretics: clorpres, tenoretic, thalitone, capozide, dyazide, hyzaar, lopressor HCT, maxzide, and prinzide.
- Loop diuretics: lasix and demadex.
- Low-potassium diuretics: aldactazide, aldactone, dyazide, and maxzide.
- Quinazoline diuretics: zaroxolyn.
- Always consult a doctor before stopping taking prescribed medications.

Step 13. Avoid muscle relaxants
Muscle relaxants are medications that are prescribed for certain types of muscle injuries. Its function as a muscle relaxant can also cause incontinence. Examples of muscle relaxants include:
- Valium, soma, flexeril, skelaxin, and robaxin.
- Sedatives can also cause incontinence.
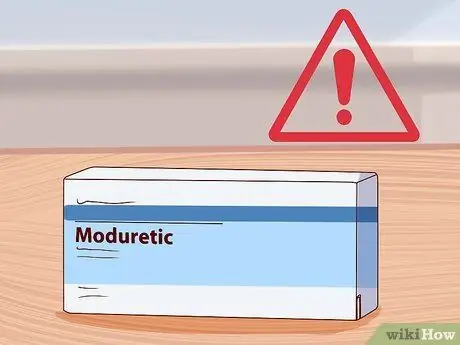
Step 14. Identify antihypertensive medications that can cause incontinence
Antihypertensive drugs are a type of medication used to lower blood pressure. This medicine may contain different types of diuretics. If you are taking antihypertensive drugs, ask your doctor for drugs that do not cause incontinence as a side effect. Examples of antihypertensive drugs are:
Moduretics, minizide, monopril HCT, and accuretics
Method 2 of 5: Treating overflow incontinence

Step 1. Find out the symptoms of overflow incontinence
Overflow incontinence results from an obstruction that “overflows” and causes incontinence. Benign prostatic hypertrophy (BPH) is the main cause of this condition because the enlarged prostate pushes and presses on the urethra as urine flows through the prostate. However, other factors can also cause these symptoms, including:
- Increased frequency of urination
- Hesitating to urinate (don't want to urinate even if you have to)
- Nocturia (going to the restroom many times at night)
- The weakening of the flow of art
- Recurrent urinary tract infections (UTIs)
- Urinary incontinence
- Urinary retention (unable to urinate at all)

Step 2. Consult a doctor
Although BPH is a major cause of overflow incontinence, there are many other factors. See a doctor and describe your symptoms to help make an accurate diagnosis.
Tumors in the bladder or prostate can also cause overflow incontinence. Therefore, most likely, your doctor will also perform an examination to rule out these factors. Tests to be performed include testing for prostate-specific antigen (PSA) on the blood, digital rectal examination (Digital Rectal Exam, DTE) to look for abnormalities in the prostate, and/or cystoscopy (a tube is inserted into the bladder through the bladder). urethra to determine the presence or absence of a tumor in it). If a tumor is found, your doctor will perform a biopsy to determine whether it is benign or malignant

Step 3. Identify medications that can cause overflow incontinence
During the consultation, your doctor will also ask about any medications you are taking as some of them may cause overflow incontinence as a side effect. Diuretics for lung disease, sedatives, and muscle relaxants are drugs known to cause incontinence. Some antidepressants, sleeping pills, and medications for high blood pressure have also been linked to overflow incontinence.
- Since many of these medications are prescribed to treat more serious illnesses than incontinence, don't stop taking them without a doctor's advice.
- Although not a drug, excessive consumption of coffee, tea, alcohol, B vitamins, and vitamin C can also cause overflow incontinence. You can request a blood panel test to determine whether or not your food contains too many B and/or C vitamins.

Step 4. Ask for medications designed to treat overflow incontinence
For mild to moderate BPH symptoms, there are several prescription drugs that can be taken to control the symptoms, including:
- Alpha blockers such as hytrin which, while not actually reducing the size of the prostate, can relieve symptoms in a matter of weeks
- 5-alpha-reductase inhibitors such as avodart that reduce prostate size without treating symptoms for six months
- Cialis which, although originally marketed to treat erectile dysfunction (ED), is capable of treating the symptoms of BPH as well
- Your doctor may prescribe a combination of avodart and hytrin to get the benefits of both. This approach is known to be safe for controlling overflow incontinence.

Step 5. Consider surgery to treat advanced symptoms
Transurethral resection of the prostate (TURP) is a procedure commonly used to clear blockages in the urinary tract caused by an enlarged prostate. This technique is performed using an endoscope that is inserted into the urethra to remove excess prostate tissue that is blocking it.
- This procedure can use lasers, microwaves, needle ablation, or photoselective evaporation. This procedure is minimally invasive and, in most cases, can be applied directly in the consulting room.
- This technique may require secondary surgery within ten years due to tissue regrowth.
Method 3 of 5: Treating Stress Incontinence

Step 1. Recognize the symptoms of stress incontinence
Stress incontinence is more often associated with leaking urine than any of the other minor symptoms associated with overflow incontinence. You can notice the leak when you laugh, cough, sneeze, run, or lift heavy objects.

Step 2. Identify the cause of stress incontinence
Excessive pressure on the bladder due to obesity or pregnancy is a major cause of stress incontinence. Stress incontinence can also occur due to a lack of muscle pressure on the bladder as a result of surgical complications. The operations commonly associated with these complications are prostate surgery and transurethral resection of the prostate.
10-20% of TURP surgeries can result in stress incontinence, with a higher percentage in patients undergoing prostate cancer surgery

Step 3. Consult a doctor
Your doctor will examine your symptoms and perform a series of tests to determine the best course of treatment for you. For patients who are obese, most likely, the doctor will also check for metabolic disorders such as thyroid disorders that can cause weight gain.

Step 4. Lose weight
If your doctor tells you that your weight is putting excess pressure on your bladder, chances are, you will be advised to lose weight.
- You should eat a healthy and balanced diet along with regular exercise. For more information, read How to Lose Weight and How to Eat Healthy.
- You should also consult a dietitian and personal trainer to develop a healthy and good weight loss plan.

Step 5. Do Kegel exercises
While Kegel exercises are commonly used to help women increase their pelvic floor muscles after childbirth, men can also do Kegel exercises to reduce stress incontinence. Do Kegels by tensing the muscles that control urination. In the beginning, you will have to practice stopping your urine in the middle of the process of excreting to know which muscles to work and to tighten.
Tighten the muscle and count from one to five before releasing it slowly while counting another one to five. Perform this exercise in three sessions, with each session consisting of ten repetitions, each day

Step 6. Consider surgical weight loss
For patients who are overweight, you may be recommended to undergo liposuction or other weight loss surgery. In one study, 71% of patients who lost more than 18 BMI (Body Mass Index) points after gastric reduction surgery were successfully cured of incontinence one year after undergoing the surgery.
Method 4 of 5: Treating Neurogenic Bladder Incontinence

Step 1. Identify causes of neurogenic bladder incontinence
The process of urination involves a series of nerves that communicate with the brain and cause the bladder and surrounding muscles to contract and relax. If you have a neuromuscular disorder-such as multiple sclerosis (MS)-you will have a disturbance in the transmission of nerve signals, resulting in a neurogenic bladder. Individuals who have had a stroke can also develop a neurogenic bladder when the muscles in the bladder that are supposed to contract and relax are affected.
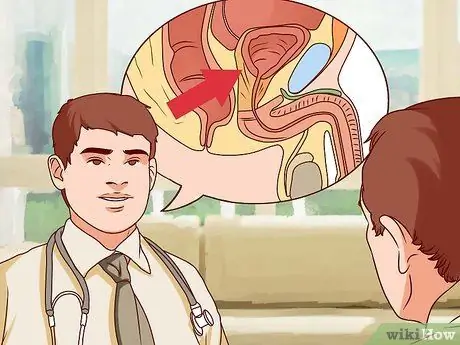
Step 2. Consult a doctor
Most people with a neurogenic bladder will recognize the causes. However, you should still consult a doctor to get a positive diagnosis. Your doctor will also provide a thorough description of the available treatment options that can be used for you.

Step 3. Try physical-psychological therapy options
Also known as periodic voiding, physical-psychological therapy combines willpower and physical exercise to help treat incontinence. This includes a combination of Kegel exercises (described in the stress incontinence section above) and avoidance notes to help you avoid episodes of incontinence before they occur.
The avoidance log is a daily track record of the fluids you consume, the amount and time you urinate, and the presence or absence of leaks. You can use these notes to help determine the best times to be near the restroom as well as times when you need to force yourself to go to the bathroom to avoid incontinence episodes
Step 4. Discuss available drug options with your doctor
While there are currently no drugs that target the bladder muscle directly to treat neurogenic bladder, some medications can reduce muscle spasms or trigger contractions. Your doctor will help determine if one or more of these medications can be effective for your condition.
Step 5. Discuss surgical options with your doctor
Various types of surgical options are now available according to your neurogenic bladder condition. In this case, your doctor will discuss:
- Electrical-stimulatory therapy that attaches electrodes and small stimulators to help deliver signals that have been disrupted by damaged nerves.
- The artificial bladder muscle consists of a ring that attaches to the base of the bladder and functions in conjunction with a special pump and valve to collect urine.
Method 5 of 5: Treating an Overactive Bladder

Step 1. Recognize the symptoms of an overactive bladder
Overactive bladder (Overactive Bladder, OAB) is a syndrome that results in an unstoppable urge to urinate as soon as possible. Common symptoms of this syndrome include:
- The urge to urinate as soon as possible
- Urge incontinence (not making it to the toilet quickly)
- High frequency of urination and nocturia (repeated urination at night)

Step 2. See your doctor
Your doctor will help you officially diagnose OAB. Since only 2% of men with OAB also experience symptoms of routine incontinence, your doctor will try to rule out other possibilities before reaching that conclusion.
- Most likely, you will have a physical exam as well as a urine analysis to test your urine. In addition, you can also be directed to undergo a cystoscopy if your condition has become quite complicated.
- Research has also shown that overactivity of the detrusor muscle, which is found in the bladder wall, plays a role.

Step 3. Use regular urination
The series of treatment includes habitual therapy with regular urinary regimens. Typically, regular voiding regimens include urinating at scheduled times-for example, once every four hours-regardless of whether you feel the urge to urinate or not.
- It is a bladder retraining regiment and a form of cognitive habit therapy. A bladder that is trained to empty its contents at certain times will prevent incontinence.
- Recent studies have shown that biofeedback-assisted habit therapy (periodic voiding) has a better effect than pharmacological therapy with oxybutinin or placebo in patients receiving treatment for detrusor instability.
- Biological feedback is done by placing electrodes on the patient to measure the subconscious subjective psychological response. In this way, the patient can clearly distinguish when the body is making a physiological response (such as an urge to urinate) and when the body is simply giving a “false response.” Thus, patients will be able to see the needs of their bodies accurately.

Step 4. Ask your doctor for available treatment options
Currently, there are various types of drugs, such as ditropan, which is dosed as 5 mg, twice a day, or 5 mg in capsules once a day. Combination therapy which includes habitual therapy, pharmacology, and biofeedback is also commonly used.






