- Author Jason Gerald gerald@how-what-advice.com.
- Public 2023-12-16 10:50.
- Last modified 2025-01-23 12:04.
Cellulitis is a skin infection that can occur when the skin is cut from a cut, scratch or injury and is exposed to bacteria. The most common types of bacteria that cause cellulitis are streptococcus and staphylococcus, characterized by a warm, red and itchy rash that spreads and fever. If not treated properly, cellulitis can lead to complications such as sepsis, meningitis or lymphangitis. Therefore, if you notice the early symptoms of cellulitis, seek immediate medical attention.
Step
Part 1 of 3: Getting a Diagnosis

Step 1. Be aware of the risk factors
Cellulitis is a skin infection that usually occurs in the lower legs or below the knees. This condition is caused by infection-causing bacteria, usually streptococcus or staphylococcus. There are several risk factors that increase the likelihood of your skin being invaded by these bacteria.
- Injury to the affected area. Cuts, burns or cuts open the skin and provide an entry point for bacteria.
- Skin conditions such as eczema, chickenpox, shingles or cracked skin from being too dry. Since the outermost layer of the skin is no longer intact, bacteria can easily enter the skin.
- Immune system disorders. If you have HIV/AIDS, diabetes, kidney disease, or another condition that impairs your immune system, you are more susceptible to skin infections.
- Lymphedema, which is chronic swelling in the arms or legs. This condition causes the skin to open, causing infection.
- Obesity has long been associated with an increased risk of developing cellulitis.
- If you've had cellulitis before, you're more likely to develop the condition.

Step 2. Understand the signs and symptoms
Cellulitis usually looks like a red, itchy rash that begins to spread over the damaged area of the skin. If you notice the rash spreading near broken, burned, or exposed skin, especially if it's on the lower legs, you may have cellulitis. Watch for the following symptoms:
- A red, itchy, warm rash that continues to spread and swell. The skin may appear tight and stretched.
- Pain, tenderness, or tenderness near the infected area.
- The onset of cold, tiredness, and fever when the infection spreads.

Step 3. Confirm the diagnosis of cellulitis
If you notice any signs of cellulitis, even if the rash hasn't spread widely, see a doctor right away. If these symptoms are left unchecked, cellulitis can lead to serious complications. Cellulitis can also be a sign of a deeper and dangerous spread of infection.
- When visiting your doctor, describe the signs and symptoms of cellulitis that you have noticed.
- In addition to performing a physical exam, your doctor may order additional tests, such as a complete blood count (CBC), or blood culture.
Part 2 of 3: Coping With Cellulitis

Step 1. Protect those close to you
MRSA (methicillin-resistant Staphylococcus aureus), ie Staphylococcus aureus bacteria that have become resistant to antibiotics, are now increasingly widespread and infectious. Do not share personal items, such as razors, towels, or clothes. Also, make sure everyone caring for you wears gloves before touching cellulitis and before touching anything that might be contaminated.

Step 2. Wash off the cellulitis on your skin
Use water and regular bath soap, then rinse thoroughly. Next, you can wrap a cool, damp towel around the cellulitis to make it more comfortable. You should still see a doctor, but washing the cellulitis will help spread the infection.

Step 3. Close the wound
You must protect the open wound until it heals. Put on a bandage and change it once a day. This will keep you protected while your body builds natural defenses.

Step 4. Wash your hands regularly
Don't let other bacteria spread to your already susceptible wound. You also don't want to risk passing the bacteria on to other open wounds on your body. Make sure you wash your hands before and after treating the wound.

Step 5. Take your regular pain medication
If the wound is painful or swollen, you can take acetaminophen or ibuprofen to reduce swelling and discomfort. Do not exceed the recommended dose. Stop taking the drug when your doctor has prescribed it.
Part 3 of 3: Treating and Preventing Cellulitis

Step 1. Take antibiotics
Antibiotics are the most commonly prescribed treatment for cellulitis. Treatment depends on the severity of the infection and your health, but usually consists of prescribing oral antibiotics that will kill the cause of the infection. The cellulitis should begin to subside within a few days and completely heal in seven to ten days.
- Your doctor may recommend that you take 500 mg of cephalexin every six hours. If MRSA is suspected, your doctor may prescribe Bactrim, Clindamycin, Doxycycline, or Minocycline. Bactrim is the most widely prescribed antibiotic for cases of MRSA.
- The doctor will ask you to come back in two or three days to report progress. If the cellulitis appears to be reducing, you should continue to take the prescribed antibiotics until they are finished (usually for 14 days) to ensure the infection is completely cured. Do not stop taking antibiotics or miss a schedule as this will make it harder for the infection to heal.
- Your doctor will prescribe oral antibiotics if you are healthy and the infection is only in the skin, but if the infection seems deeper and you are also experiencing other symptoms, oral antibiotics may not clear up quickly enough.
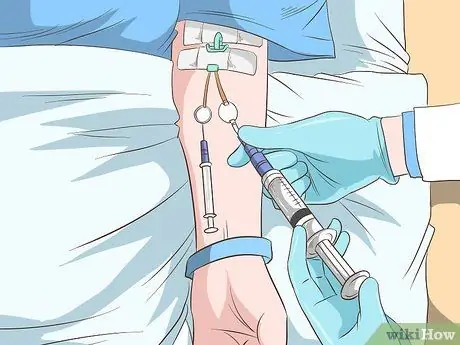
Step 2. Get treatment for severe cellulitis
In extreme cases of cellulitis that has progressed deeper, you may need to stay in the hospital. Antibiotics will be given intravenously or by injection to treat the infection more quickly than oral antibiotics.

Step 3. Clean the wound carefully
Cellulitis most often occurs when the wound is not treated properly so that it is open and easily infected with bacteria. The best way to prevent this is to clean the skin immediately the second your skin is cut, scratched, or burned.
- Wash the wound with soap and water. Continue washing every day until healed.
- If the wound is large or deep, cover it with a sterile bandage. Change the bandage daily until it heals.

Step 4. Lift your legs
Inadequate blood circulation can slow healing, but removing the area affected by cellulitis can help. If cellulitis occurs in the legs, you can elevate the legs to improve blood circulation and speed healing.
Try placing your feet on some pillows while you sleep
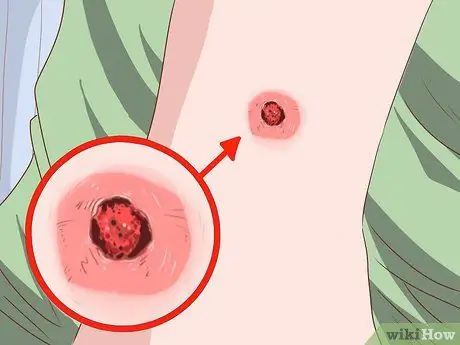
Step 5. Monitor the wound for signs of infection
When removing the bandage daily, check to make sure the wound is healing properly. If the sore starts to swell, becomes red, or itchy, you should seek medical attention. If the wound is oozing fluid, that's also a sign of a possible infection, so make an appointment with your doctor right away.

Step 6. Keep your skin healthy
Because cellulitis usually occurs in people with skin diseases, maintaining healthy skin is very important as a preventive measure. If you have sensitive or dry skin, or have diabetes, eczema, or another disorder that affects the skin, use the following techniques to prevent sores and cellulitis.
- Use moisturizer to prevent chapped skin and drink plenty of water to keep your body hydrated.
- Protect your feet by wearing sturdy socks and shoes.
- Trim your toenails carefully so as not to injure the skin.
- Treat fungal infections in the feet so they don't become more severe infections.
- Treat lymphedema to prevent chapped skin.
- Avoid activities that cause cuts and scrapes to the legs and feet (such as hiking in the thorns, gardening, and so on).
Tips
- Make sure you return to see your doctor after treatment. In severe cases, you should see a specialist such as an infectious disease specialist.
- You can prevent cellulitis from reappearing by protecting your skin. You should always clean any cuts or scrapes on your skin with soap and water. You should also always cover the injured skin with a bandage or plaster.






