- Author Jason Gerald [email protected].
- Public 2023-12-16 10:50.
- Last modified 2025-01-23 12:04.
Human papillomavirus (HPV) represents more than 100 different types of viruses that may be transmitted through sexual contact (also known as sexually transmitted diseases/STDs). HPV is one of the most common types of sexually transmitted diseases and is transmitted through direct contact with mucous membranes in the genital area. In fact, about 80% of women have had the infection at some point in their lives. Several types of viruses cause genital warts to appear in both men and women. In addition, there are also viruses that trigger cervical cancer and other cancers in women that are less popular, such as cancer of the vagina, anus, and vulva. Today, HPV can also trigger throat cancer in men and women, you know! Given the enormous potential for harm, everyone needs to learn to recognize the symptoms of HPV in order to get information about how to treat or treat it. In general, some types of HPV can be diagnosed independently, but some need to be examined and diagnosed by a medical professional!
Step
Method 1 of 4: Detecting Symptoms

Step 1. Identify the presence or absence of warts that are a symptom of low-risk HPV
The obvious evidence that accompanies low-risk HPV is genital warts. Generally, genital warts are shaped like small red bumps, flat lesions, or small bumps on the skin. Genital warts also generally appear in groups, and will appear within a few days or weeks after infection occurs.
- In women, genital warts are most common on the vulva and labia, but they may also appear around the anus, vagina, or cervix.
- The series of low-risk HPV viruses can also trigger the appearance of lesions around the cervix, although in general they will not develop into cancer cells.
Step 2. Learn how to detect high-risk HPV
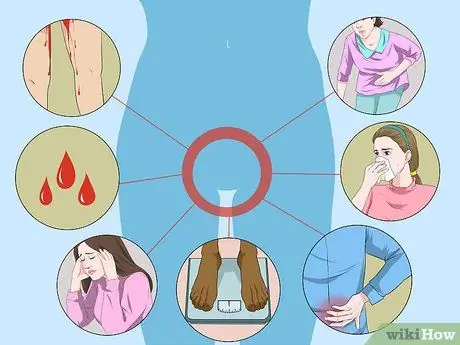
High-risk HPV is very rarely accompanied by specific symptoms, unless it has transformed into advanced cancer. To prevent this, you should have an annual pelvic exam at your gynecologist to detect potential problems before they progress to precancerous or even cancerous stages. Symptoms of advanced HPV that have the potential to develop into cervical cancer are:
- Inconsistent bleeding or spotting in the middle of a menstrual period/after sexual intercourse.
- Irregular menstrual cycle.
- Fatigue.
- Weight loss or loss of appetite.
- Pain in the back, legs, or pelvis.
- Swelling of one leg.
- Discomfort in the vaginal area.
- Bad-smelling discharge from the vagina.

Step 3. Detect potential other cancers
High-risk HPV is the most common viral category that causes cervical cancer, but is often associated with cancers in the vulva, anus, and throat area. These types of cancer can be detected early on through a routine health check-up process. That's why, you should start getting used to regular health checks to the doctor!
- Try palpating areas that are exposed from the outside, such as the vulva and anus, to check for lumps that may be genital warts.
- If you think you have HPV, contact your obstetrician or general practitioner immediately, and ask them to detect the presence or absence of potential cancers associated with HPV.
Method 2 of 4: Detecting HPV Types

Step 1. Get tested to determine the type of HPV you have in your body
In general, HPV manifests in more than 100 different types of viruses. Of the many types, about 40 of them are transmitted through sexual contact, while 60 other viruses can trigger the appearance of warts in areas such as the hands and feet.
- The HPV virus that is not sexually transmitted generally enters your body through skin-to-skin contact or open sores on the skin, and may be represented by the appearance of warts around the infected area.
- The HPV virus that is transmitted through sexual contact will enter your body through direct genital contact or skin-to-genital contact. Meanwhile, HPV infection around the mouth or upper respiratory tract may also be caused by oral sex. This type of HPV virus is usually represented by the appearance of warts, or even not accompanied by any symptoms. That is why, a medical examination is needed by a doctor to diagnose the existence of the HPV virus that is transmitted through sexual intercourse more accurately.

Step 2. Consider the possibility of contracting HPV through sexual intercourse
Generally, the HPV strains that are transmitted through sexual contact will fall into two broad categories: high-risk HPV and low-risk HPV.
- About 40 types of HPV are transmitted through direct contact with mucous membranes, such as those around your genital area. These types are most commonly transmitted through sexual intercourse.
- The high-risk HPV strain is transmitted through sexual contact and has been more closely associated with serious health problems, such as cancer. Included in it are HPV 16, 18, 31, 33, 45, 52, 58, and several other types of viruses. The most common types of HPV that develop into cervical cancer are 16 and 18. That's why, the two types of viruses are the most commonly tested because 70% of cervical cancers are caused by it. Medical examination is mandatory for those of you who have high-risk HPV viruses.
- The low-risk HPV strains are HPV 6, 11, 40, 42, 43, 44, 53, 54, 61, 72, 73, and 81. HPV 6 and 11 are the most common forms of the low-risk category of HPV, and the most common associated with genital warts. Low-risk HPV so rarely transforms into cancer that it is not part of the routine screening of patients.
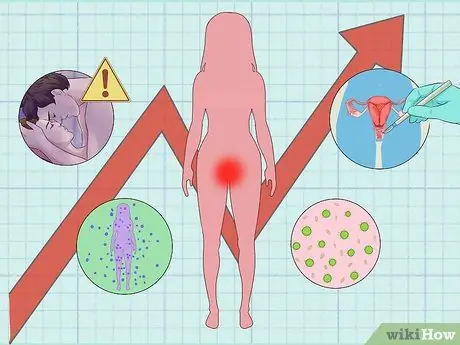
Step 3. Evaluate the risks you have
Several factors can increase a woman's risk of contracting HPV. For example, HPV transmission factors will increase in women who have more than one sexual partner, have a low immune system due to HIV or other immune diseases, are undergoing cancer treatment, and engage in unprotected sexual activity.
Remember, the risk factors above are only indicators that indicate the possibility of transmission. Thus, you are not necessarily infected with HPV if you have one or more of these risk factors
Method 3 of 4: Doing Medical Treatment
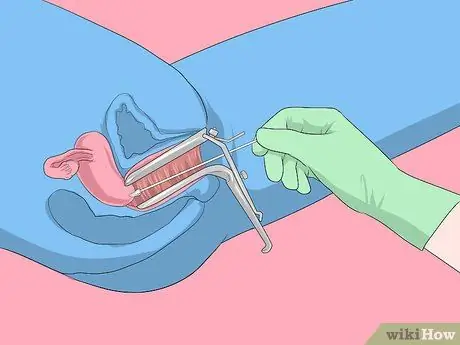
Step 1. Perform the Pap smear procedure
The Pap smear is the primary method commonly used by doctors to identify precancerous changes in the cervix or the risk of cervical cancer. If the results are inconsistent, your doctor may ask you to do an HPV DNA test to get a positive diagnosis of the HPV virus. In some cases, the doctor will perform both types of examinations at the same time.
Women under 65 years of age should have a Pap smear procedure every three years, if previous Pap smear results were normal. If not, your doctor will recommend a more specific schedule for your problem

Step 2. Perform an HPV test in addition to the pap smear procedure
HPV screening is not part of the routine health screening of women. However, many doctors will perform these tests in addition to the pap smear procedure, especially if the patient has relevant concerns. In general, the sampling procedure for the HPV test is no different from the Pap smear, which involves taking fluid from the inside of the cervix.
- HPV screening is generally only recommended for women over the age of 30 so it may not be recommended by doctors to younger patients.
- HPV is common in young women, and most viruses can be "cured" by a good immune system before they develop into serious complications. In addition, the doctor may also ask you to do other tests, such as a pap smear, to determine whether or not there are other problems that need to be diagnosed further.
- At this stage, a new HPV test was developed that was effective for female patients. That is why, women cannot ask their male partners to check their risk for the HPV virus to the doctor.

Step 3. Perform a medical examination of the warts that appear
If you notice any warts, lesions, or lumps appearing around the genital area, call your doctor immediately! Ask your doctor for help to check for any suspicious symptoms or conditions as soon as possible.
- Generally, genital warts will heal on their own. Although it really depends on the symptoms you experience, most likely your doctor will only ask you to monitor the condition of the warts on a regular basis without the need for specific treatment.
- Generally, the treatment methods recommended by doctors are the use of topical ointments or the procedure of freezing the warts. Try asking if the treatment procedure you can do yourself at home, or should be done with the help of a medical professional.
- If you are currently on treatment for genital warts, try asking your doctor, "What should I do to minimize the risk of infection in this area and reduce the risk of warts reappearing in the future?"

Step 4. Have an annual medical check-up at the doctor
At this point, share any concerns you have about HPV. Generally, HPV examination includes checking the condition of the vulva, vagina, and anal. If you feel you are at risk for contracting an HPV infection, convey the suspicion to your doctor so that these areas can be examined.
Method 4 of 4: Preventing HPV Infection
Step 1. Put on a condom
If used correctly, condoms are a contraceptive that has 97% effectiveness to ward off most sexually transmitted diseases. Therefore, always wear a condom before vaginal and/or anal penetration, and also wear extra protection such as a dental dam before having oral sex. Tips for wearing a condom correctly:
- Make sure the surface of the condom is not torn or has holes. Also, read the expiration date. Never use an expired or damaged condom!
- Slowly, open the condom wrapper so that the latex layer does not tear.
- Take a condom and pinch the tip before attaching it to the base of the penis.
- Still pinching the tip of the condom with one hand, straighten the condom with the help of the head of the penis, and use your other hand to lower the surface of the condom to the base of the penis.
- After use, tie the open end of the condom, then throw it in the trash.

Step 2. Get vaccinated against HPV
Now, vaccines to protect men and women and the HPV strain are widely available and you can access at any time. In general, women are advised to get vaccinated at the age of 11-12 years. However, the HPV vaccine can still be given between the ages of 9 and 26 years. Meanwhile, men should vaccinate at the age of 11 or 12 years, or until the age of 21 years.
- It is recommended that the HPV vaccination be carried out before a woman is sexually active, but it will still be beneficial for young women who are already sexually active.
- The HPV vaccine is generally given three times over six months.

Step 3. Discuss your sexual history
Before having sex with a new partner, try to have an honest and open discussion about each other's previous sexual history. On this occasion, share any tests you have recently had, and the number of sexual partners you have had since your last checkup.
- Take time to discuss your sexual history before having sex with a new partner.
- Don't be afraid to ask specific questions like, "Have you ever had symptoms that might be related to HPV such as genital warts?" and “How many sexual partners have you had?”
- Respect the decision of others to keep their personal information private. However, also understand that you have no obligation to have sex with anyone. In other words, you may refuse to have sexual intercourse with penetration if you have not received the necessary information.
Tips
- Most sexually active men and women will develop an HPV infection at some point in their lives. However, most forms of infection will clear up on their own before symptoms or complications worsen.
- The best way to avoid HPV is to practice abstinence. In particular, abstinence is the perfect choice for those of you who aren't really sure about actively engaging in any form of sexual intercourse.
- In America, about 1% of sexually active adults can develop genital warts at any time.
Warning
- HPV can infect areas that are not protected by a condom.
- In fact, certain populations have a higher risk of developing cancers caused by HPV, such as gay and bisexual men, and people with weakened immune systems (including people with HIV/AIDS).






