- Author Jason Gerald gerald@how-what-advice.com.
- Public 2024-01-19 22:11.
- Last modified 2025-06-01 06:05.
Experts say that the bladder can drop from its normal position in the pelvis if the pelvic floor becomes very weak or because there is too much pressure there. When the pelvic floor weakens, the bladder presses against the vaginal wall, and this condition is called a descending bladder (cystocele). Research shows that as many as 50% of women experience a drooping bladder after pregnancy. So, it's a fairly common problem. If you're concerned about having a descending bladder, talk to your doctor as there are a variety of treatment options available.
Step
Part 1 of 4: Recognizing Symptoms of Descending Bladder

Step 1. Feel the bulge of tissue in the vagina
In serious cases, you may feel your bladder drop into your vagina. When sitting, it feels like sitting on a ball or egg, but the feeling disappears when standing or lying down. This is the most common symptom of a cystocele, and you should see your GP or gynecologist as soon as possible.
This feeling is generally considered a sign of a severe cystocele

Step 2. Watch for pain or discomfort in the pelvic area
If you have pain, pressure, or discomfort in your lower abdomen, pelvis, or vagina, see a doctor. There are a number of conditions that cause these symptoms, including a drooping bladder.
- If the bladder is drooping, this pain, pressure, or discomfort will get worse when you cough, sneeze, work hard, or put pressure on the pelvic floor muscles. If this is the case, tell your doctor.
- If your bladder is going down, you may also feel as if something is coming out of your vagina.

Step 3. Consider urinary symptoms
If you tend to pass urine when you cough, sneeze, laugh, or work hard, you have a condition called "stress incontinence." Women who have given birth are especially prone to this condition, and a drooping bladder is sometimes the main cause. See a doctor to solve the problem.
- Also pay attention to changes in urination, such as difficulty passing urine, bladder not completely emptying after urinating (also known as urinary retention), and increased frequency and urgency to urinate.
- Also keep in mind whether you have frequent bladder infections, or urinary tract infections (UTIs). The definition of “frequently” here is experiencing more than one UTI within six months. Women with cystocele conditions will usually have frequent bladder infections. So, pay attention to the frequency of your UTI.

Step 4. Don't ignore pain during sex
Pain during penetration is called dyspareunia and is triggered by a number of physical conditions, including a drooping bladder. If you have dyspareunia, see your GP or gynecologist as soon as possible.
If you are experiencing pain during intercourse, and you have just given birth vaginally, the most likely cause is a drooping bladder. Don't delay seeing a doctor

Step 5. Monitor back pain
Some women who have a cystocele also experience pain, pressure, or discomfort in the lower back. Back pain is a very common symptom that can mean anything, or is not serious at all. However, it is best to schedule an appointment with your doctor. This will be especially important if you are also experiencing other symptoms.

Step 6. Know that some women have no symptoms at all
If your case is mild, you may not feel any of the above symptoms. Several new cases of cystocele were discovered in routine gynecological examinations.
- However, if you show or experience any of the above symptoms, immediately consult a GP or gynecologist.
- If you have no symptoms, usually no treatment is needed.
Part 2 of 4: Understanding the Causes of a Dropping Bladder

Step 1. Recognize that pregnancy and childbirth are the most common causes of a drooping bladder
During pregnancy and childbirth, the pelvic muscles and their supporting tissues are stressed and stretched. Because there are muscles that hold the bladder in place, pressure or weakness there can cause the bladder to fall into the vagina.
Women who have been pregnant, especially multiple vaginal deliveries, have a higher risk of developing a cystocele. In fact, women who give birth by cesarean section are also at risk

Step 2. Consider the effects of menopause
Postmenopausal women are at high risk of bladder drooping due to reduced levels of the female sex hormone, estrogen. Estrogen plays a role in maintaining the strength, firmness, and endurance of the vaginal muscles. The lack of estrogen levels that accompanies the menopausal transition makes muscles thinner and inelastic, and results in overall weakness.
Be aware that this drop in estrogen levels occurs even if you are menopausal through artificial means, such as with surgical removal of the uterus (hysterectomy) and/or ovaries. This surgery not only damages the pelvic area, but also changes estrogen levels. Therefore, even if you are younger than most postmenopausal women and healthy, you are still at risk for a cystocele

Step 3. Recognize that intense stress is also a contributing factor
Intense tension or lifting heavy objects can sometimes trigger the bladder to drop. When straining the muscles in the pelvic floor, there is a risk of triggering a cystocele (especially if the vaginal wall muscles have weakened due to menopause or childbirth). The types of tension that can cause a cystocele are:
- Lifting very heavy objects (including children)
- Chronic and intense cough
- Constipation and straining during bowel movements

Step 4. Consider your weight
If you are overweight or obese, your risk of bladder dropping also increases. The extra weight puts additional stress on the pelvic floor muscles.
Being overweight or obese can be determined by the body mass index (BMI), which is an indicator of body fat. The BMI formula is weight in kilograms (kg) divided by height squared in meters (m). A BMI of 25-29.9 is overweight, while a BMI over 30 is considered obese
Part 3 of 4: Diagnosing Descending Bladder

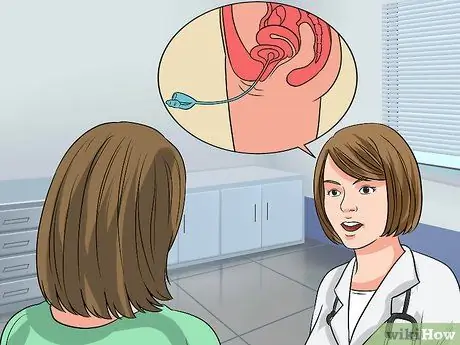
Step 1. Make an appointment with the doctor
If you think you have a drooping bladder, schedule an appointment with your GP or gynecologist.
Prepare as much information as possible to share with your doctor, including a complete medical history and a detailed description of your symptoms

Step 2. Perform a pelvic exam
As a first step, the doctor may perform routine gynecological examinations. In this examination, a cystocele is detected by placing a speculum (an instrument for examining the inside of the body) against the posterior (back) wall of the vagina while you are lying down with your knees bent and your ankles supported. Your doctor will ask you to strain (such as when pushing a baby in labor or to have a bowel movement) or to cough. If you have a cystocele, your doctor will see or feel a soft lump protruding into the anterior (inner) wall of your vagina when you push.
- A bladder that falls into the vagina is considered a positive diagnosis of a descending bladder.
- In some cases, in addition to performing a standard pelvic exam, your doctor may need to examine you while you are standing. This is useful for evaluating the descent of the bladder from different positions.
- If the doctor notices the bladder dropping against the back wall of the vagina, they will also perform a rectal exam. This examination will help the doctor determine muscle strength.
- You don't need to prepare anything for this examination and the process doesn't take long. You may feel a bit uncomfortable during the exam, but for many women this is just a routine checkup just like a pap smear.
Step 3. Go for follow-up if you have bleeding, incontinence, or sexual dysfunction
Your doctor will suggest a test called a cystometric or urodynamic test.
- Cystometric studies measure how full your bladder is when you first feel the urge to urinate, when your bladder feels "full," and when your bladder is completely full.
- The doctor will ask you to urinate in a container connected to a computer, which will take several measurements. Then, you will have to lie on an examining table and the doctor will insert a thin, flexible catheter into your bladder.
- Urodynamics is a series of tests. This test includes metered urination (or uroflow), which calculates how long it takes you to start urinating, how long it takes to pass urine to finish, and how much urine you pass. This test also includes cystometry as mentioned above. In addition, you will also undergo a discharge or discharge phase test.
- In most urodynamic tests, the doctor will place a thin, flexible catheter into the bladder, which will remain there during urination. Special sensors will collect data that will be interpreted by doctors.
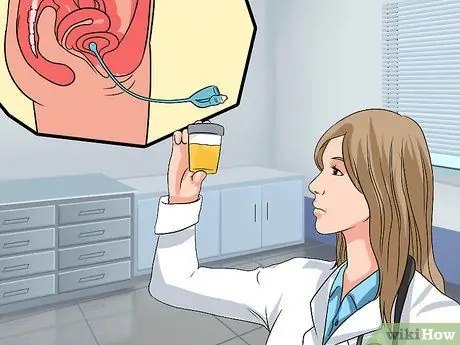
Step 4. Talk to your doctor about additional tests
In some cases, usually when the cystocel case is more severe, the doctor may suggest additional tests. These additional tests generally include:
- Urinalysis. In a urinalysis, your urine will be tested for signs of infection (such as a UTI). The doctor will also test the bladder to see if it is completely empty. The trick is to insert a catheter into the urethra to drain and measure the amount of urine remaining after urination, residue after urination or post-void residual (PVR). A PVR of more than 50-100 milliliters is a diagnosis of urinary retention, one of the symptoms of a drooping bladder.
- Ultrasound with PVR. The ultrasound test sends sound waves that bounce off the bladder and back into the ultrasound machine, and in the process produce an image of the bladder. This image also shows the amount of urine remaining in the bladder after urination, or voiding.
- Voiding cystourethrogram (VCUG). In this test, the doctor takes X-rays during urination (voiding) to view the bladder and evaluate for problems. The VCUG displays the shape of the bladder and analyzes urine flow to determine possible blockages. This test can also be used to diagnose stress urinary incontinence overshadowed by a cystocele. Both of these diagnoses should be made as the patient will also need incontinence procedures in addition to cystocele repair (if surgery is required).

Step 5. Get a specific diagnosis
Once the doctor confirms that the bladder is descending, you should ask for a more detailed diagnosis. Cystocele is divided into several categories based on its severity. The best treatment depends on the type of cystocele itself, as well as the symptoms it causes. Descending bladder conditions are divided into the following “grades”:
- Grade 1 is a mild case. For Grade 1 cystocele, only part of the bladder descends into the vagina. You may feel mild symptoms such as mild discomfort and bedwetting, but some women do not show any symptoms. Treatment is Kegel exercises, rest, and avoiding heavy lifting or straining. If you are already menopausal, estrogen replacement therapy may be considered.
- Grade 2 is a moderate case. In Grade 2 cystocele, the entire bladder descends into the vagina. The fall may be so far that it touches the vaginal opening. Symptoms of discomfort and incontinence progress from mild to moderate. Surgery to repair a cystocele may be necessary, but you can treat symptoms with a vaginal pessary (a small plastic or silicone device that is placed inside the vagina to hold the vaginal wall where it should be).
- Grade 3 is a severe case. In the case of a Grade 3 cystocele, part of the bladder protrudes from the vaginal opening. Symptoms such as discomfort and urinary incontinence become severe. Surgical repair of the cystocele and/or pessary as in the case of Stage 2 is also required.
- Stage 4 is a case of complete cystocele. If you have a Grade 4 cystocele, the entire bladder falls in and out of the vaginal opening. In this case, you may experience other, more severe problems, such as a descending uterus and rectum.
Part 4 of 4: Coping With a Dropping Bladder

Step 1. Assess whether you need treatment
Grade 1 descending bladder usually does not require medical treatment because it is not accompanied by pain or discomfort. Ask if your doctor recommends medical treatment right away or if you just "see the progress" first. If your symptoms don't bother you too much, your doctor may suggest basic treatments such as Kegel exercises and physical therapy.
- Note that your doctor may recommend that you stop certain activities, such as lifting weights or other activities that put a strain on your pelvic muscles. However, regular exercise remains healthy.
- You should also know that the effect of symptoms on quality of life is a key factor in deciding on treatment. For example, your bladder condition is severe, but you are not bothered by the symptoms. In this case, you can consult a less intense treatment option. On the other hand, it may be that your condition is mild, but your symptoms are causing significant disturbances or problems. So talk to your doctor about a more aggressive approach.

Step 2. Do Kegel exercises
Kegel exercises are performed by tightening the pelvic floor muscles (as when you are trying to stop the flow of urine), holding them briefly, then relaxing them. By doing this exercise regularly, which doesn't require any special equipment and can be done anywhere (including while waiting in line, sitting at your desk, or relaxing on the couch), your pelvic muscles will become stronger. In mild cases, Kegel exercises can prevent the bladder from descending further. Here's how to do Kegel exercises:
- Tighten your pelvic floor muscles, which are the muscles used to stop the flow of urine when you urinate.
- Hold for five seconds, then release for five seconds.
- Try to hold for ten seconds.
- The goal is to do 3 to 4 sets of 10 reps each day.

Step 3. Use a pessary
A pessary is a small silicone device that is inserted into the vagina to hold the bladder (and other pelvic organs) in place. Some pessaries are specially made for standalone use, but some have to be inserted by a doctor. There are various shapes and sizes of pessaries, and a healthcare professional can help you choose the most suitable one.
- Pessaries can be uncomfortable at times, and some women have a hard time keeping them from falling. It can also cause vaginal ulceration (if the size is not correct) and infection (if not regularly removed and cleaned once a month). You will need a topical estrogen cream to prevent damage to the vaginal walls.
- Despite these drawbacks, pessaries are a useful alternative, especially if you want to delay or are not a good candidate for surgery. Talk to your doctor, and weigh the pros and cons for your case.

Step 4. Try estrogen replacement therapy
Since a drop in estrogen levels often results in weakening of the vaginal muscles, your doctor may recommend estrogen therapy. Estrogen can be given as a pill, vaginal cream, or ring that is inserted into the vagina in an effort to strengthen weak pelvic floor muscles. The cream is not very absorbent so it is strongest on the applied area.
Estrogen therapy also carries risks. Women with certain types of cancer should not take estrogen, and you should discuss the potential harms and benefits with your doctor. In general, topical estrogen treatments are less risky than “systemic” estrogen treatments
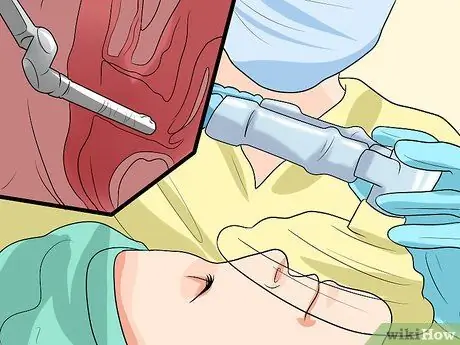
Step 5. Run the operation
If other treatments don't work or the cystocele is very severe (Grade 3 or 4), your doctor may suggest surgery. The surgery options may not be for everyone. For example, if you are planning to have children, it may be a good idea to postpone surgery until the desired family member is complete to avoid the bladder dropping again after delivery. Older women have a higher risk of surgery.
- The most common surgical procedure for a descending bladder is a vaginoplasty. The surgeon will lift the bladder back into place, then tighten and strengthen the vaginal muscles to make sure everything is in its proper place. There are other surgeries to consider, and your doctor will suggest the procedure he thinks is best for your situation.
- Prior to surgery, the surgeon will explain the procedure and all the risks and benefits, as well as possible complications. Potential complications include UTI, incontinence, bleeding, infection, and in some rare cases, damage to the urinary tract requiring surgical repair. In addition, there is a possibility of irritation or feeling of pain during sexual intercourse after surgery because there are stitches or scar tissue in the body.
- You will need local, regional, or total anesthesia, depending on the case. Many patients are able to go home within one to three days after surgery, and most are able to return to their normal activities within six weeks.
- If the uterus is also descending, the doctor may suggest a hysterectomy to remove it. This procedure can be done at the same time as surgery. If the cystocele is also accompanied by stress urinary incontinence, a concomitant urethral suspension procedure may be required.






