- Author Jason Gerald gerald@how-what-advice.com.
- Public 2024-01-19 22:11.
- Last modified 2025-01-23 12:04.
A miscarriage, also known as a “spontaneous abortion,” occurs when a pregnancy fails to develop before 20 weeks of gestation. Miscarriage is common, afflicting nearly 25 percent of known pregnancies. Determining whether or not you had a miscarriage is difficult because some of the same symptoms occur in a healthy pregnancy. Follow all doctor's advice if you have a miscarriage.
Step
Part 1 of 2: Miscarriage Causes and Symptoms
Step 1. Understand why miscarriages happen
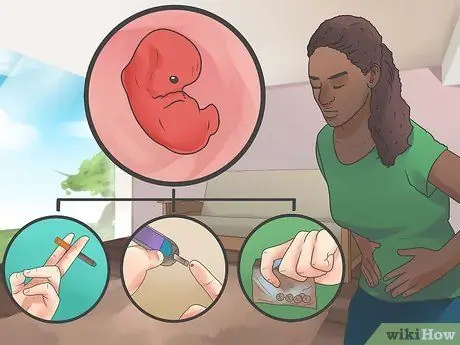
Miscarriage most often occurs in the early weeks of pregnancy. Chromosomal abnormalities are the most common cause, and in most cases, there is nothing pregnant women can do to prevent them. The risk of miscarriage decreases after the thirteenth week of pregnancy. By this time, most chromosomal abnormalities will have ended the pregnancy. The following factors increase the risk of miscarriage in pregnant women:
- Older women have a higher risk. Women between the ages of 35 and 45 have a 20-30 percent chance of having a miscarriage. And women over 45 have a 50 percent chance.
- Women with a severe chronic disease, such as diabetes or lupus.
- Abnormalities in the uterus, such as the presence of scar tissue.
- Smoking, drug use, and alcohol consumption.
- Women who are overweight or underweight.
- Women who have had more than one miscarriage.

Step 2. Check for vaginal bleeding
Heavy vaginal bleeding is the most common sign of a miscarriage. This bleeding is accompanied by the same cramping as during menstruation. The blood that comes out is usually brown or bright red.
- Spotting and light bleeding can also occur in a healthy pregnancy. Heavy bleeding accompanied by the discharge of clots may indicate a miscarriage. Tell your doctor if you experience bleeding during pregnancy.
- According to the American Pregnancy Association, 50 to 75 percent of miscarriages are chemical pregnancies. That is, a miscarriage occurs immediately after implantation. Often the woman does not realize that she is pregnant and she experiences bleeding during her normal monthly period. The bleeding may be heavier than usual and the cramping may be more severe.

Step 3. Check for vaginal mucus
One of the symptoms of miscarriage is the discharge of pink-white vaginal mucus that may contain pregnancy tissue. If the discharge looks like lumpy or solid tissue, this may be a sign that a miscarriage is or has occurred. You should immediately consult a doctor.
- Most pregnant women experience increased vaginal discharge that is clear or milky white called Leukorrhea or vaginal discharge. So if the level of discharge is high, you don't need to worry.
- It's also possible that you may mistake the urine for spotting as vaginal discharge. Urinary incontinence (loss of bladder control resulting in urine leakage/wetting) is a common occurrence in healthy pregnancies.

Step 4. Watch for aches and pains
Pregnancy usually causes a variety of aches and pains. In the case of a miscarriage, pain is usually felt in the lower back, and can vary from mild to severe. If you experience lower back pain, tell your doctor immediately.
- The stabbing and pain that sometimes occurs in the abdomen, pelvis, and back is often the result of the body adjusting to accommodate the growing fetus. If the pain is severe, prolonged, or occurs in waves, you may have miscarried, especially if it's accompanied by bleeding.
- You can also feel “real contractions” if you have a miscarriage. Contractions last every 15 to 20 minutes, and the pain is often excruciating.

Step 5. Analyze your pregnancy symptoms
Pregnancy has many different symptoms, all of which are caused by increased hormone levels in the body's system. If your symptoms subside, it could be a sign that a miscarriage has occurred and that your hormone levels are returning to their pre-pregnancy state.
- If you've had a miscarriage, your levels of morning sickness will decrease, your breasts will shrink and become tender, and you'll no longer feel like you're pregnant. In a healthy pregnancy, these early symptoms often go away on their own by 13 weeks of gestation, a time when the risk of miscarriage also decreases.
- The appearance and severity of symptoms varies with each pregnancy. Sudden changes that occur before the thirteenth week need to immediately consult a doctor.

Step 6. Visit a doctor to be sure
Go to the doctor, emergency room, or poly gynecologist at the hospital to get a definitive answer as to whether you had a miscarriage. Even if you feel all of the above symptoms, there is still a chance that the fetus will survive, depending on the type of miscarriage.
- Depending on the age of your pregnancy, the doctor's examination may include a blood test, pelvic exam, or ultrasound to check the continuity of the womb.
- If you have heavy bleeding in early pregnancy, your doctor probably won't tell you to come to the clinic unless you can.
Part 2 of 2: Miscarriage Treatment

Step 1. Know the different types of miscarriage
Miscarriage affects every woman's body in somewhat different ways. In some cases, all of the uterine tissue breaks down and leaves the body quickly, while in other cases the process takes longer and is more difficult. Here are some types of miscarriage and their effects on the body:
- Threat of miscarriage: cervix remains closed. It may be that the bleeding and other miscarriage symptoms have stopped, and the pregnancy continues as normal.
- Definite miscarriage: heavy bleeding occurs and the cervix begins to open. At this point, the pregnancy is unlikely to continue.
- Incomplete miscarriage: some of the uterine tissue is shed from the body, but some is left inside. Sometimes there is a procedure that must be done to remove the remaining tissue.
- Complete miscarriage: all uterine tissue shed and out of the body.
- Missed abortion: even though the pregnancy has ended, the tissue still remains in the body. Sometimes it comes out on its own and sometimes it takes a certain procedure to get it out.
- Ectopic pregnancy (pregnancy outside the uterus): Technically this is not a type of miscarriage, but a type of pregnancy failure. Instead of implanting in the uterus, the egg is implanted in the fallopian tube or in the ovary, where it is not possible for the fetus to grow.

Step 2. Call your doctor immediately if the bleeding stops on its own
If you have heavy bleeding that eventually subsides, and this occurs early in your pregnancy, you don't need to go to the hospital. Many pregnant women prefer not to go to the hospital and just rest at home. Usually this is not a problem, as long as the bleeding stops within 10 days to 2 weeks.
- If you experience cramping or other pain, your doctor can give you suggestions to make you feel more comfortable during a miscarriage.
- If you want to determine whether a miscarriage has occurred, have an ultrasound checked.

Step 3. Go to the doctor immediately if the bleeding does not stop
If you have heavy bleeding and other miscarriage symptoms, and you're not sure whether the miscarriage was complete or incomplete, your doctor will usually use the following strategies:
- Natural management: You just wait for the remaining tissue to come out and the bleeding stops on its own.
- Medical management: Treatment is given to remove the remaining tissue from the body. The patient has to stay in the hospital for a while. Bleeding afterward can last up to three weeks.
- Surgical management: Dilation and curettage, known as D&C (Dilation and Curettage), is performed to remove the remaining tissue. Bleeding usually stops faster than the use of medical management methods. Medication is usually given to slow the bleeding.

Step 4. Watch for symptoms
If the bleeding continues after the time limit stated by the doctor, seek medical attention immediately. If you experience other symptoms such as chills or fever, go to the doctor or hospital immediately.

Step 5. Seek grief counseling
Losing a fetus at any stage can result in emotional trauma. You need time to grieve the loss. Seek counseling to help. Ask your doctor for references to grief counseling, or make an appointment with a therapist in your area.
- There is no definite time when you will feel better, because this is different for every woman. Give yourself as much time to grieve as needed.
- When you're ready to get pregnant again, talk to your doctor about making an appointment with a high-risk pregnancy specialist. This action only needs to be done by women who have had two or more miscarriages.






