- Author Jason Gerald gerald@how-what-advice.com.
- Public 2023-12-16 10:50.
- Last modified 2025-01-23 12:04.
Lazy eye disease, also known as amblyopia, usually develops in early childhood and affects about 2-3% of the pediatric population. Amblyopia often runs in families. This condition is treatable if detected early, but can lead to vision loss if left untreated. Although in some cases the symptoms of lazy eye are obvious, sometimes they can be difficult to spot in other children. The child himself may not even be aware he is experiencing it. You should immediately consult an ophthalmologist as early as possible to diagnose and treat amblyopia. You can use several techniques to determine if your child has lazy eye, but you should always consult an eye professional (especially one who has been specially trained to treat children's eyes).
Note: this article is primarily intended for readers living in the US. Some adjustments, such as locating an optometrist, may be necessary if you do not live in the US.
Step
Method 1 of 6: Looking for the Symptoms

Step 1. Understand the causes of lazy eye
Amblyopia occurs when the brain has trouble communicating with the eyes in the correct way. This condition may occur when one eye has better focusing power than the other eye. Amblyopia can be difficult to detect alone because it doesn't cause any visual or shape changes to the eye. The only way to accurately diagnose lazy eye is to visit an ophthalmologist.
- Strabismus is the main cause of amblyopia. Strabismus is a disorder in the arrangement of the eyes, which is either directed inward (esotropia), outward (exotropia), upwards (hypertropia), or downwards (hypotropia). This condition is sometimes referred to as “cross-eye.” Ultimately, the "straight" eye dominates visual signals to the brain, resulting in a medical condition known as "strabismic amblyopia. However, not all lazy eye disease is associated with strabismus.
- Amblyopia may also occur due to a structural problem, such as a droopy eyelid.
- Other problems with the eye, such as cataracts (the “cloudy” spot in the eye) or glaucoma, can also cause lazy eye. This type of amblyopia is called “deprivation amblyopia” and must be treated surgically.
- Some differences in refraction in each eye can also result in amblyopia. For example, some people are farsighted in one eye and farsighted in the other (a condition known as anisometropia). The brain will choose one eye to use and ignore the other eye. This type of amblyopia is called “refractive amblyopia.”
- Sometimes, bilateral amblyopia can affect both eyes. For example, a baby may be born with cataracts in both eyes. A healthcare professional can diagnose and provide treatment options for this type of amblyopia.

Step 2. Look for common symptoms
Your child probably won't complain about his vision. Over time, a person with amblyopia may get used to the state of one eye being more visually sharp. A professional eye exam is the only way to determine if your child has lazy eye. However, there are symptoms of their own that you can look for.
- Poor depth perception. Your child may have difficulty analyzing depth (stereopsis) and viewing 3D movies. Your child may have trouble seeing distant objects, such as a blackboard at school.
- Cockeye. If your child's eyes seem to be in the wrong position, then he or she may have strabismus, which is a common cause of amblyopia.
- Squints, eye rubbing, and tilting of the head are routine for your child. All of these may be symptoms of blurred vision, which is a common side effect of the condition amblyopia.
- Your child becomes angry or restless when you cover one eye. Some children can experience this if you cover one of their eyes. This may be a sign that their eyes are not sending balanced visual signals to the brain.
- Children have difficulty at school. Sometimes, a child may have difficulty learning due to amblyopia. Talk to your child's teacher and ask if your child makes excuses when asked to read from a distance (eg: “I have a headache” or “My eyes are itchy”).
- You should seek the help of an ophthalmologist to check for squint or vision problems in children younger than 6 months of age. At this age, your child's eyesight is still developing so much that the tests you do at home may not be as effective.

Step 3. Perform a movable object test
Watch your child's response to movement to see if one eye responds more slowly than the other. Look for a ballpoint pen with a light-colored lid or other brightly colored object. Ask your child to focus on a specific point on the object (such as the cap of a pen or the round part of a lollipop).
- Ask your child to focus on the same part while following the movement of the colored object with his eyes.
- Move the object slowly to the right and left. Then, move it up and down. Watch your child's eyes carefully as you move the object. Notice if one eye appears to be slower than the other in following the movement of objects.
- Cover one eye of the child and move the object again: left, right, up, and down. Cover the other eye and repeat the test.
- Record the response of each eye. This will help you determine if one eye is moving more slowly than the other.

Step 4. Do a photo test
If you believe your child's eyes are crossed, it's time to have an eye exam. Doing this will give you time to analyze so you can look for signs that may indicate a problem with your child's eyes. This is especially useful with infants and young children, who usually find it difficult to keep still when you want to examine their eyes.
- You can use existing photos if they show the eye in clear detail. If you don't have photos that match, ask someone to help you take new ones.
- Use the reflection of a small ballpoint pen to determine if you have lazy eye. Ask an assistant to hold this small flashlight pen at a distance of about 90 cm from your child's eyes.
- Ask the child to see the light.
- When the light hits your child's eyes, take a picture of his eyes.
-
Look for symmetrical reflections of light in your child's iris or pupil.
- If the light is reflected at the same point in each eye, then your child's eyes are most likely straight.
- If the light reflection is at an asymmetrical point, then one eye may squint inward or outward.
- If you're not sure, take a few shots to check your child's eyes again.

Step 5. Perform an open-close test
This test can be done on children aged 6 months or older. An open-close test can help determine if their eyes are flush in place and working in the same capacity.
- Have your child sit facing you or on someone's lap. Cover one eye with a wooden spoon.
- Ask your child to look at a toy with his eyes open for a few seconds.
- Open closed eyes and see the response. Check to see if the eye is moving backwards because the focus is distorted. This movement can indicate a problem that should be checked by an eye doctor.
- Repeat the test on the other eye.
Method 2 of 6: Visiting a Professional Ophthalmologist

Step 1. Locate the pediatric ophthalmologist
A pediatric ophthalmologist is a medical doctor who specializes in pediatric eye care. While all ophthalmologists can treat pediatric patients, those with specializations are better trained to look for abnormalities in the eyes of children.
- Search online to find a pediatric ophthalmologist in your area. In the US, The American Optometric Association has a search feature that can help you find an optometrist in your area. The American Association for Pediatric Ophthalmology and Strabismus also has a doctor finder app. You may have to find a pediatric ophthalmologist in your area yourself. Use search engines for help.
- If you live in the suburbs or a small town, you may have to search the nearest town to find an eye specialist.
- Ask for recommendations from friends and family with children. If you know people who have children with vision problems, ask them to recommend an eye doctor. Doing this will help you determine whether or not the doctor will be the right choice for you.
- If you have health insurance, make sure you choose the services of a medical professional that will be paid for by your insurance policy. If you are unsure, you can contact your insurance company to verify if they will pay for the eye doctor you are considering.
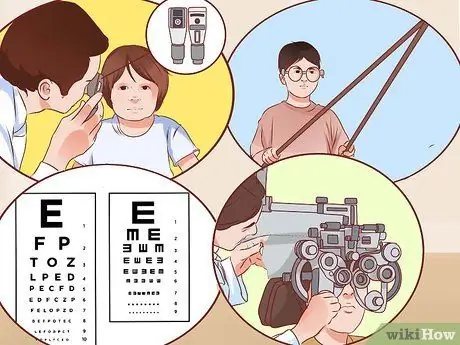
Step 2. Familiarize yourself with some test and examination equipment
A professional ophthalmologist will examine your child's vision and eye condition to determine whether he has lazy eye condition or not. Understanding this will help you feel more comfortable when you visit your eye doctor. You will also help your child feel calmer.
- Retinoscopy. The doctor may use a handheld device called a retinoscope. This tool is useful for examining the eyes. The retinoscope will shine a light into the eye. As the light rays move, doctors can determine refractive abnormalities (eg farsightedness, farsightedness, astigmatism) in the eye by observing the "red reflex" portion of the retina. This method can also be very useful for diagnosing tumors or cataracts in infants. Your doctor will likely use eye drops to examine your child this way.
- Prism. Your doctor may use a prism to check the light reflex in your child's eye. If the reflexes are symmetrical, then the eyes are normal; if not, then your child may have strabismus (which can be the cause of amblyopia). The doctor will hold the prism in front of one eye and adjust it to read the eye reflex. This technique is not as accurate as other strabismus tests, but may be necessary when examining very young children.
- Visual acuity assessment testing (VAT). This type of test includes several types of examinations. The most basic VAT tests use the familiar “Snellen chart,” which requires your child to read the smallest letters they can see on a standard letter diagram. Other tests may include tests for light response, pupillary response, ability to follow the movement of objects, color blindness tests, and distance vision tests.
- Photoscreening. Photoscreening is used in vision examinations by ophthalmologists. This method uses a camera to check for vision problems such as strabismus and refractive errors, by analyzing the light reflex of the eye. Photoscreening is especially useful in very young children (under 3 years/toddlers), children who find it difficult to sit still, and children who are noncooperative or nonverbal (cannot communicate with words), such as those with autism. This test usually takes less than a minute.
- Cycloplegic refraction test. This test determines how the structure of the eye displays and receives images from the lens. The ophthalmologist will use eye drops to perform this test.

Step 3. Tell your child about the benefits of a visit to the doctor
Young children may be afraid of new situations, such as a doctor's examination. Telling them what will happen during the eye exam can help them feel more calm and comfortable. You can also tell them to act appropriately during the inspection. If possible, make sure your child is not hungry, sleepy, or thirsty when you take him to the eye doctor, as these can make him restless and more difficult to examine.
- The doctor will likely use eye drops to moisten your child's eyes. This will help determine the extent of the refractive error in his vision during the examination.
- Doctors use flashlights, light pens, or other lighting devices to help them monitor the light reflex in their child's eyes.
- The doctor may use objects and photographs to measure your child's eye motility and misplacement.
- The doctor may use an ophthalmoscope or other similar equipment to check for any disease or abnormal conditions in your child's eyes.

Step 4. Make sure your child is comfortable with the eye doctor
If your child has vision problems, he or she may have to spend a lot of time in the doctor's office (or, at least, time that seems long to the child). Children who wear glasses should have their eyes checked at least once a year. The ophthalmologist and your child must have a good relationship.
- You should always feel that the doctor cares about your child. If the ophthalmologist you have selected is unwilling to answer questions and communicate with you, find another ophthalmologist.
- You should not feel pressured or harassed by any doctor. If you have to wait a very long time, feel pressured to make an appointment, or feel the doctor sees you as a nuisance, don't be afraid to find another doctor. You may find a doctor who can better answer your needs.
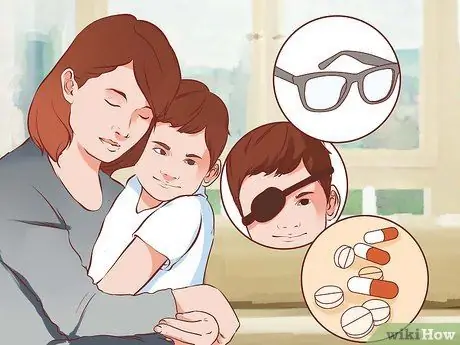
Step 5. Learn about different treatments
After examining your child's eyesight, the ophthalmologist can suggest the right treatment for your child. If the doctor has determined that your child has lazy eye, treatments may involve glasses, eye bandages, or eye medications.
The doctor may also recommend eye surgery to correct the position of the eye muscles. This procedure is performed under general anesthesia. The child will be sedated. A small incision will be made in the eye, and an eye muscle will be lengthened or shortened, depending on the need as needed to correct lazy eye problems. The eye may still need a bandage afterwards
Method 3 of 6: Treating Lazy Eyes
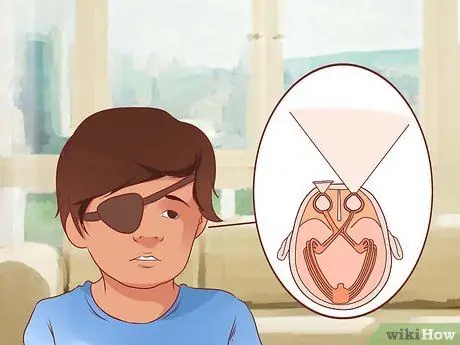
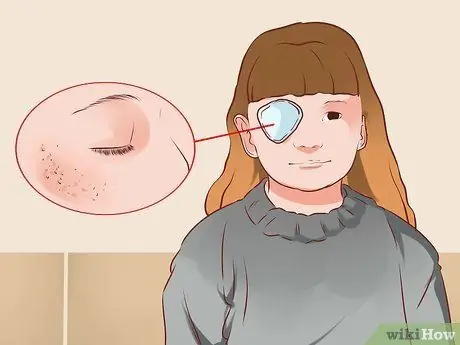
Step 1. Place a bandage/cover over the healthy eye
Once the cause of the amblyopia is determined, closure is usually the recommended treatment for forcing the brain to see with the weaker eye. For example, if surgery has succeeded in correcting vision problems such as refractive amblyopia, eye closure may still be needed for a while, to force the brain to recognize visual signals that were previously ignored.
- Request an eye patch sample from your doctor. For this method to work, the blindfold must cover the entire eye. Your eye doctor can confirm the correct size.
- You can choose an eye patch with an elastic band or an eye patch with an adhesive substance.
- The Amblyopia Kids Network has written an analysis of various blindfolds, as well as information on where to buy them. Look for information on where to buy in your area or ask an eye doctor for recommendations.

Step 2. Have your child wear an eye patch for 2-6 hours a day
In the past, parents were advised to have their children wear a blindfold at all times, but recent studies have shown that children can improve their eyesight by wearing a blindfold for at least 2 hours a day.
- Your child may have to gradually increase the use of the eye patch over the time recommended by your doctor. Start with 20-30 minutes, 3 times a day. Gradually increase the time until your child can wear the blindfold for the recommended amount of time each day.
- Older children and children with severe amblyopia may need to wear eye patches for longer periods of time each day. Your doctor can advise when and how long your child should wear the eye patch.

Step 3. Check for eye improvement
Blindfolding can give results in just a few weeks. However, sometimes you also have to wait a few months to see the results. Check for improvement by re-testing your child's eyes monthly (or according to the routine recommended by your ophthalmologist).
- Continue monthly checkups as lazy eye conditions usually begin to improve after 6, 9, or 12 months of treatment. Response times will vary depending on each child (and how honest he is in wearing the blindfold).
- Ask your child to continue wearing the blindfold as long as you notice any changes.

Step 4. Perform activities that require hand-eye coordination
Forcing the weak eye to work harder while the stronger eye is covered will make your child's treatment more effective.
- Involve the child in art activities that include coloring, painting, connecting the dots, or cutting and gluing.
- Look at pictures in children's story books and/or read with your child.
- Have your child focus on the details in the illustration or read the words in the story.
- Be aware that your child's level of depth perception will be reduced by wearing a blindfold, so the game of catch and throw may be a little difficult for him.
- For older children, there are various video games developed to help their eye coordination. For example, software developer Ubisoft, which has partnered with McGill University and Amblyotech to produce games like “Dig Rush” to treat amblyopia. Ask your eye doctor if this game could be an option for your child's treatment.
Step 5. Stay in touch with your eye doctor
Sometimes, eye treatments don't give you the results you expect. Your professional ophthalmologist is the right person to determine this. Children are usually able to adapt to various situations. Keeping in touch with your ophthalmologist will ensure that you are aware of new options that may be available to treat your child's eyes.
Method 4 of 6: Considering Other Treatments

Step 1. Ask your doctor about atropine
Atropine may be an option if your child is unable or unwilling to wear an eye patch. Drops of atropine will obscure vision and can be used in the "good" eye to force the child to wear the "bad" eye. Atropine does not hurt the eyes like other eye drops.
- Some studies suggest that eye drops are as effective or more effective than eye patches in treating amblyopia. Part of the effect may be that the use of eye drops poses a lower risk of social stigma for children than if they wear an eye patch. Thus, children are more likely to be more prepared to cooperate with this method of treatment.
- These eye drops may not need to be used during the eye patch.
- Atropine eye drops have side effects, so do not use them without consulting your child's ophthalmologist first.

Step 2. Consider the Eyetronix Flicker Glass treatment
If your child's amblyopia is refractive, flicker glass treatment can be an effective treatment alternative. Flicker glass glasses resemble sunglasses. It works by alternating clear and “foggy” (blurred) vision at the frequency prescribed by your eye doctor. These glasses may be a good choice for older children, or children who don't respond to other treatments.
- This method of treatment works most effectively for children with mild to moderate anisometropic amblyopia (eg amblyopia caused by two eyes with different strengths).
- Eyetronix Flicker Glass treatment is usually completed in 12 weeks. This treatment may not be effective if your child has tried eye patch treatment for amblyopia before.
- As with other alternative treatments, make sure you always consult your child's ophthalmologist before trying any treatment.
Step 3. Consider using RevitalVision to treat amblyopia
RevitalVision uses a computer to stimulate specific changes in your child's brain to improve their vision. This computer treatment (which takes an average of 40 minutes in 40 sessions) can be done at home.
- RevitalVision can be very useful for older amblyopia patients.
- You should consult your doctor to purchase RevitalVision.
Method 5 of 6: Caring for the Eye Area

Step 1. Watch the eye area
The eye area may become irritated or infected during closure. Pay attention to the area in your child's eyes. If you notice spots or welts around your eyes, consult your doctor or ophthalmologist to find out how to treat them.
Step 2. Reduce irritation
Eye patches, whether elastic or adhesive, can irritate the skin around the eyes and cause a mild rash. If possible, choose an eye patch with a hypoallergenic adhesive to reduce the risk of skin discomfort.
Nexcare manufactures a variety of eye patches with hypoallergenic adhesives. Ortopad manufactures hypoallergenic eye patches, both adhesive and eyeglass-like coverings. You can also consult your pediatrician for advice

Step 3. Adjust the size of the eye patch
If the skin under the glue patch is irritated, try covering the area around the eye that is larger than the flap with gauze. Attach the gauze to the child's face with medical tape. Then, attach the blindfold to the gauze.
You can also try trimming off some of the adhesive on the eye patch so that less of the area touches the skin. The trick here is to make sure your child's normal eye is still completely closed and the blindfold fits properly

Step 4. Try an eye patch that can be attached to the glasses
Because the eye patch like this will not directly touch the skin, the problem of irritation will be prevented. This eye patch can be a good choice if your child has very sensitive skin.
An eye patch attached to the glasses can provide good coverage over the weak eye. However, you may have to attach a side panel to the glasses to prevent your child from seeing through the eye patch

Step 5. Treat the skin
Clean the area around the eyes with water to remove any traces of irritants that may remain when the eye patch is removed. Apply an emollient or moisturizer to the affected area to help keep the skin moisturized. Both of these substances will help the skin repair itself and protect the skin from the risk of inflammation in the future.
- Skin creams or ointments can reduce inflammation, but you should follow the instructions carefully and not overuse these products. In some cases, the best treatment is to do nothing and just allow the skin to "breathe."
- Consult a medical professional for advice on care for your child's irritated skin.
Method 6 of 6: Providing Support to Children with Lazy Eyes

Step 1. Explain what happened
For eye patch treatment to be successful, your child must wear the patch for the recommended time. He will agree more easily if he understands why he needs the blindfold.
- Explain how an eye patch can help your child and what might happen if he doesn't wear it. Tell your child that wearing an eye patch will make his eyes stronger. Tell him that if he doesn't wear it, his eyesight may deteriorate (but don't scare him).
- If possible, ask your child for input on how much time to use the "eye patch" each day.

Step 2. Ask family members and friends for support
Communication is key to helping your child feel comfortable wearing the blindfold. Children who feel embarrassed or have low self-esteem when wearing an eye patch will have a harder time completing their treatment successfully.
- Ask those around your child to empathize with him and support him, so he can get through the treatment period to completion.
- Tell your child that he has several people he can turn to if he has a problem. Be open when answering the questions. Tell your family and friends why you are blindfolded so they can support your child too.

Step 3. Talk to your child's teacher or daycare center
If your child must wear a blindfold to school, explain the situation to the instructor or supervisor.
- Discuss so that your child's teacher can explain to classmates why your child should wear a blindfold, and how they should support it. Ensure that school and faculty staff are aware that bullying of the use of blindfolds should not be tolerated.
- Discuss if there are any academic adjustments your child can make while wearing the blindfold. For example, ask if teachers can give your child more difficult assignments first, provide tutorials, offer work plans, and/or monitor student progress on a weekly basis. All of these things can help your child feel more comfortable with their eyes closed and maintain good performance in school.

Step 4. Provide a sense of comfort
Despite your best efforts, other children may make fun of or make hurtful comments to your child. Listen to your child as this happens, reassure him and reassure him that this treatment is only temporary and the results will be worth it.
- You can consider wearing an eye patch as well as a form of loyalty to your friend. Even if it's just a few times, your child may find it less awkward to see that adults can wear blinders too. You can also put blindfolds on your child's dolls.
- Get your child to see the blindfold as a game rather than a punishment. Even if your child understands that the blindfold is necessary for a good reason, he may take it as a punishment. Tell him that pirates and other cool characters wear blinders. Suggest that your child compete against himself to keep the blindfold on.
- There are several children's books that discuss blindfolds. Take My New Eye Patch, A Book for Parents and Children, for example, which uses photos and stories to explain what it's like to wear an eye patch. Reading about other people's experiences can help your child feel normal while wearing the blindfold.

Step 5. Develop a reward system
Prepare a gift plan for your child when he puts on the blindfold without complaining or trouble. Rewards can help keep your child motivated to wear a blindfold (remember, younger children don't understand the concept of rewards and long-term consequences).
- Hang a calendar or whiteboard to monitor your child's progress.
- Give small gifts like stickers, pencils, or small toys when your child has crossed certain stepping stones, such as wearing an eye patch every day for a week.
- Use gifts as a distraction for very young children. For example, if your child removes the blindfold, replace it and give your child a toy or other gift to distract him from the blindfold.

Step 6. Help your child adjust on a daily basis
Each time your child puts on an eye patch, it takes the brain about 10 to 15 minutes to adjust to the strong eye being closed. Lazy eye occurs when the brain ignores the line of sight from one eye. The blindfold will force the brain to detect the neglected pathway. This experience can be scary for children who are not used to it. Spend time with your child to calm him down.
Do something fun at a time like this to help make the transition easier. Creating positive associations between blindfolding and a pleasurable experience can make it easier for your child to go through the blindfold process

Step 7. Get creative
If your child's blindfold uses an adhesive type, allow your child to decorate the outside of the blindfold with stickers, markers, or glitter. Ask your doctor for advice about the best type of decoration to use and how to decorate it safely.
- Never decorate the inside of the blindfold (the side facing the eye).
- Design sites like Pinterest offer a wide variety of decorating ideas. Prevent Blindness also offers eye patch decoration suggestions.
- Consider having a decorating party. You can give extra blindfolds to your child's friends so they can decorate it. This can help your child feel less isolated when he wears the blindfold.
Tips
- Use the techniques in this article with professional eye care. Do not attempt to diagnose and treat lazy eye without consulting an ophthalmologist or pediatric ophthalmologist.
- Always maintain open communication between you and your child. Also keep in touch with your eye doctor. Ask your doctor if you have any questions.
- If your child's eyes are crossed, share this with photographers so they can position your child in a way that makes his lazy eye invisible in the photo. This can help your child feel less insecure when he has to provide photos, such as on “photograph” days at school or for the yearbook.
Warning
- If lazy eye is present from birth, then other health conditions may occur in the uterus at the same time. Make sure you consult your pediatrician thoroughly to check if he has any other medical conditions.
- If you notice any unusual side effects, take your child to an emergency facility immediately or call your doctor.
- All eye problems should be examined by an ophthalmologist or pediatric ophthalmologist. Early detection and treatment are important to prevent vision loss.
- If lazy eye is not treated, then the child may experience vision loss, ranging from mild to severe.






